Shocking Findings: Vaccine-Preventable Diseases Could Be Deteriorating the Health of Older Adults in the U.S.
2024-10-25
Author: Wei Ling
Introduction
In the U.S., adults aged 50 and older are facing an alarming threat from vaccine-preventable diseases (VPDs) such as influenza, pneumococcal disease, and herpes zoster. Recent findings indicate that these diseases not only result in short-term illness but also lead to severe long-term health consequences that are often overlooked. This retrospective analysis aims to uncover the startling downstream effects of VPDs on hospitalized adults and the implications for public health and vaccination strategies.
Understanding the Burden of VPDs
The burden of VPDs on adults aged 50 and above represents a significant public health crisis, costing approximately $26.5 billion annually in direct medical expenses alone. The Centers for Disease Control and Prevention (CDC) reports that a staggering 70-85% of influenza-related deaths and 50-70% of hospitalizations occur among those aged 65 and older. The repercussions of VPDs extend beyond immediate health issues; they can exacerbate existing chronic conditions and lead to increased morbidity and mortality.
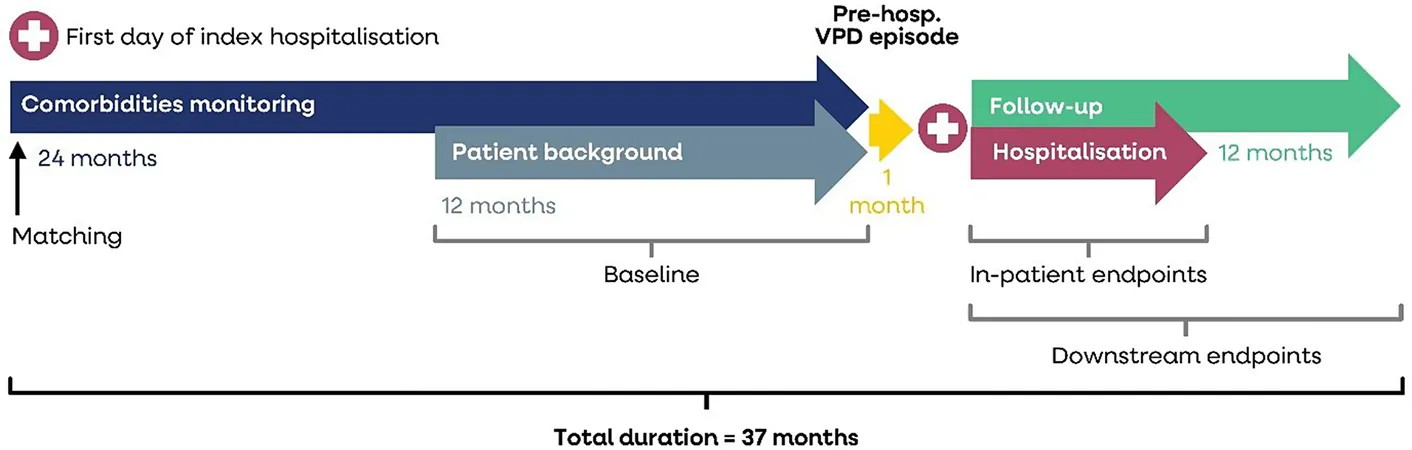
Study Methodology
Conducted from 2016 to 2019, this retrospective observational study utilized hospital claims data to analyze health outcomes in adults hospitalized with a VPD diagnosis compared to matched controls. The focus was on various outcomes, including mortality rates, changes in the Charlson Comorbidity Index (CCI) score, new diagnoses of comorbidities, and loss of independence—a critical aspect seldom discussed when considering the impacts of vaccination.
Results: A Grim Reality
The analysis revealed harrowing statistics: patients admitted with a VPD faced death rates that were shockingly higher than those without VPDs, with a 4.08 times greater risk within 30 days of hospitalization and a 2.76 times greater risk at one-year follow-up.
Additionally, 65-86% of adults diagnosed with a VPD developed new comorbidities within a year, compared to only 13-41% of their non-VPD counterparts. The mean increase in CCI scores—a widely recognized measure of overall health—was significantly greater among VPD cases (3.23) compared to controls (0.89).
Furthermore, the study exposed a troubling trend regarding independence: 41% of patients with VPDs lost their ability to live independently post-hospitalization, a stark contrast to only 12% of controls needing help. This was illustrated by increased requirements for home health care and transfers to long-term care facilities.
The Bigger Picture
These findings emphasize the magnitude of the healthcare crisis posed by VPDs among older adults. The connection between VPDs and new comorbidities, not only exacerbates existing health issues but also diminishes quality of life, leading to more complex healthcare needs.
Call to Action: Increase Vaccination Awareness
This study raises urgent concerns about the current state of adult vaccination in the U.S. The immune responses of older adults can significantly wane, increasing their vulnerability to infections that can settle into chronic health issues. Despite this, vaccine uptake remains low, greatly underestimating the consequences of VPDs on overall mortality and health outcomes.
The call is clear: We need to enhance awareness among healthcare providers, policymakers, and, importantly, the public about the critical importance of adult vaccination. By elevating the conversation regarding the implications of VPDs on morbidity and mortality, we can combat this public health crisis more effectively.
Conclusion
The repercussions of vaccine-preventable diseases in hospitalized adults are vast and deeply concerning. As the healthcare system grapples with an aging population and rising rates of comorbidities, understanding the extensive impact of VPDs will be crucial to developing effective vaccination policies and, ultimately, saving lives. The time for urgent action on vaccination is now—before more lives are lost and health deteriorates further within our older adult population.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)