New Study Reveals Surprising Rise in Day Three Parasitaemia After Treatment for Malaria in Ethiopia
2025-03-18
Author: Nur
In-Depth Report: A Concerning Trend Post-Treatment
In a groundbreaking study conducted in Arbaminch Zuria, Ethiopia, researchers have discovered troubling findings concerning the treatment of uncomplicated Plasmodium falciparum malaria. Following administration of artemether-lumefantrine (AL) combined with a single dose of primaquine (PQ), a significant 17% of patients still exhibited detectable levels of malaria parasites by Day 3 post-treatment. This revelation raises urgent questions about potential emerging resistance to malaria treatments in the region.
Study Overview: An Insight Into Treatment Efficacy
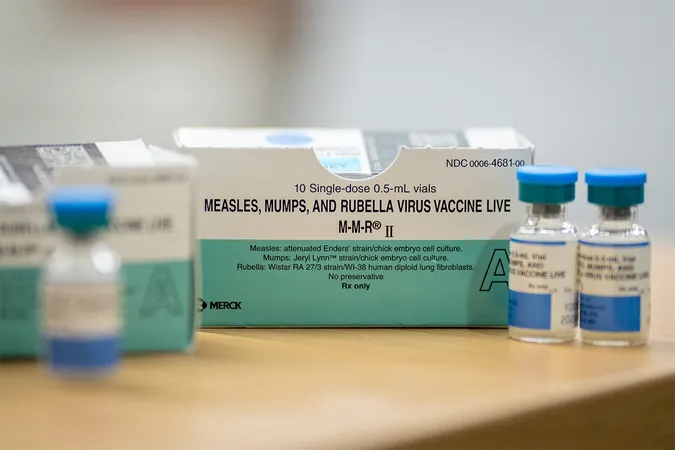
Since 2017, AL has been Ethiopia's first-line treatment for uncomplicated P. falciparum malaria, bolstered by the addition of primaquine to combat the transmission of gametocytes—the stages of the parasite responsible for spreading malaria to mosquitoes. The World Health Organization emphasizes the necessity of ongoing efficacy monitoring of malaria treatments to adapt response strategies effectively.
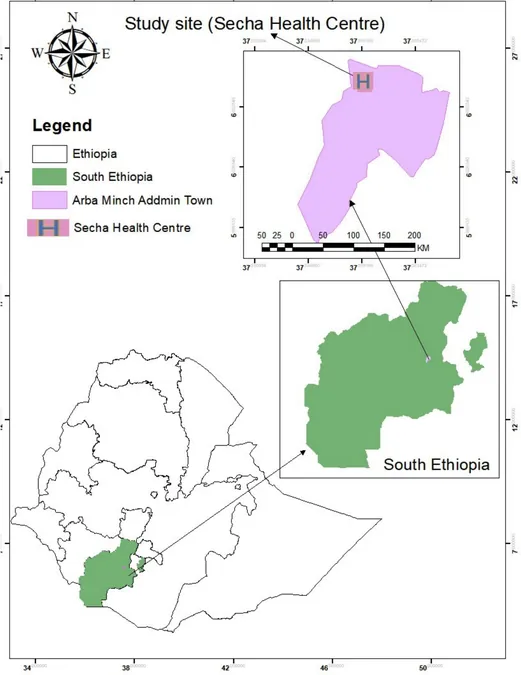
The study, conducted from October 2023 to January 2024 at Shecha Health Centre, involved 93 participants aged six months and older with confirmed uncomplicated malaria. Following treatment, patients were monitored for 28 days to evaluate both clinical outcomes and the presence of parasites. Impressively, overall cure rates were reported at 96.6% uncorrected and a perfect 100% when considering corrected data. Yet, the unsettling discovery of persistent parasitaemia in nearly one-fifth of participants by Day 3 cannot be ignored.
The Bigger Picture: Assessing Malaria’s Global Impact
Globally, malaria continues to claim hundreds of thousands of lives annually. In 2023 alone, an estimated 263 million cases were reported worldwide. With P. falciparum responsible for the majority of malaria fatalities in Africa, the stakes are high. Ethiopia faces a significant burden, with an estimated 70% of cases attributed to this deadly species.
Malaria’s tendency to evolve and develop resistance necessitates constant vigilance. Various studies in Ethiopia have indicated that while AL remains effective, certain areas are now reporting signs of resistance, prompting health agencies to recommend bi-annual efficacy assessments in all endemic regions.
Key Findings: Efficacy Versus Resistance
The persistence of parasites on Day 3 is significant; research shows that more than 10% of patients still harbor parasites at this juncture suggests partial resistance. While this finding starkly contrasts initial expectations, it aligns with emerging patterns of drug resistance observed in East Africa.
It's vital to note that even though AL exhibits rapid efficacy in clearing the blood stage of malaria, the drug's ability to eliminate mature gametocytes remains limited. Thus, the addition of primaquine plays a critical role, as evidenced by the 100% clearance of detected gametocytes by Day 3—an essential outcome for intervention strategies in controlling transmission.
Conclusion and Call to Action
As we dissect these revelations, it becomes clear that while the efficacy of AL plus primaquine remains robust—providing hope in the fight against malaria—the emergence of treatment failure indicators emphasizes an urgent need for strategic action. Continued monitoring and timely adaptations of treatment protocols in Ethiopia are essential to curtail the rising tide of resistance and maintain progress against one of the world’s deadliest diseases.
The clock is ticking as the quest to eliminate malaria progresses amidst a backdrop of evolving challenges. The implications of this study resonate beyond Arbaminch, necessitating a unified response to safeguard public health against the looming threat of drug resistance.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)