Unlocking the Link Between Cognitive Decline, Brain Changes, and Suicide Risk in Older Adults
2025-09-03
Author: Jacques
Understanding the Study's Foundation
This groundbreaking research explores the complex relationship between cognitive impairment, white matter hyperintensities (WMH), and suicide risk in older adults suffering from late-life depression (LLD). Conducted with a focused group of 58 elders aged 65 and above, the study categorizes participants into three distinct groups: those with recent suicide attempts, non-suicidal peers, and healthy controls.
Who Were the Participants?
Participants hailed from various backgrounds, with 'Group 1' comprising individuals from psychiatric units who had recently attempted suicide. These cases, referred by a specialized Suicide Prevention Center, emphasized the urgency of care required for these vulnerable patients. 'Group 2' included depressed patients who had never engaged in self-harm, while 'Group 3' consisted of healthy older adults free from any psychiatric illness.
Research Methodology: A Strict Approach
To ensure validity, the study implemented rigorous inclusion and exclusion criteria. All participants completed a variety of cognitive and psychiatric assessments, including the Cognitive Abilities Screening Instrument (CASI) and the Mini-Mental State Examination (MMSE), ensuring a comprehensive evaluation of their mental health status.
Unveiling the MRI Findings
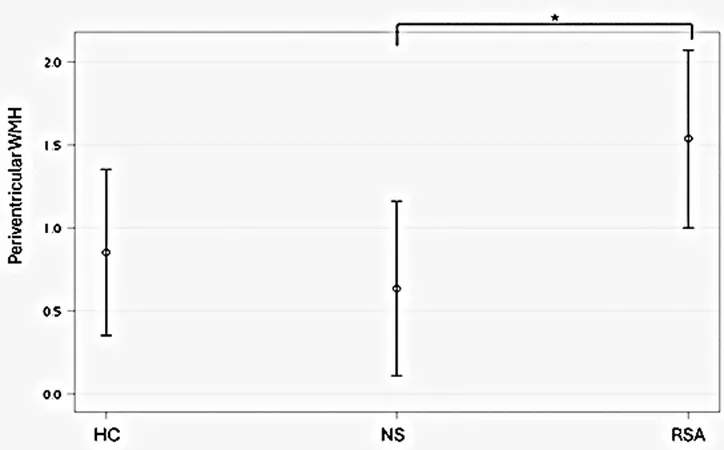
Using advanced imaging technology, researchers employed MRI scans to assess brain changes, specifically looking at WMH. The study’s findings revealed that participants with a history of suicide attempts displayed significantly higher levels of WMH, particularly in the periventricular areas, suggesting a potential biomarker for suicide risk.
Key Discoveries: Cognitive Function at Risk
Notably, those with recent suicide attempts exhibited lower overall cognitive scores, especially in attention and orientation tasks. This finding suggests a troubling link between cognitive decline and increased susceptibility to suicidal behaviors in older adults.
Implications for Future Research
While the findings shed new light on the connections between cognitive deficits, WMH burden, and suicide risk, researchers emphasize the need for further studies. The exploratory nature of this study, paired with its limited sample size, calls for deeper investigations into the neuropsychological underpinnings of these relationships.
Why This Matters
As the population ages, understanding these dynamics becomes increasingly critical. Identifying potential early warning signs of cognitive decline and suicidal ideation could lead to better prevention strategies, ultimately saving lives. This study not only advances scientific knowledge but also poses a clarion call for increased awareness and targeted intervention among healthcare providers working with older adults.
The Bigger Picture
As we unravel the interconnections between brain health, mental illness, and suicide in older adults, we uncover the urgent need for refined assessment tools and tailored therapeutic approaches. Only by addressing these complexities can we hope to mitigate the heartbreak of suicide in our aging population.








 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)