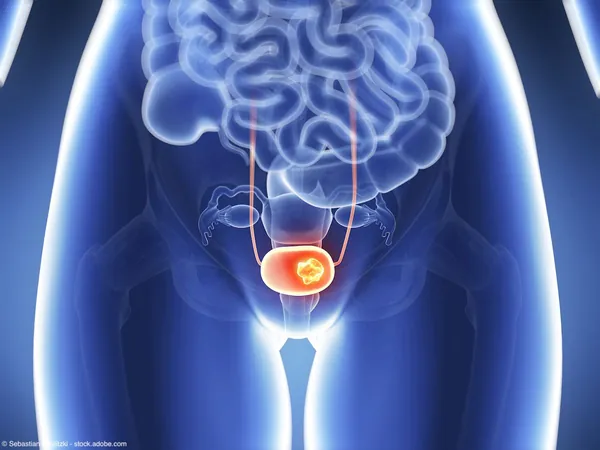
Unveiling the Urgent Need for Innovative Treatments in Plasmacytoid Urothelial Carcinoma
2025-01-17
Author: Siti
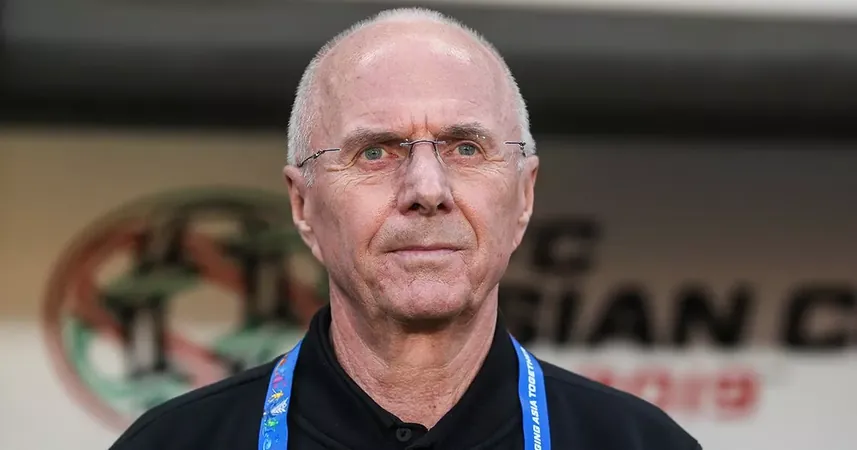
In a pivotal interview, Dr. Fed Ghali, an assistant professor of urology at the Yale School of Medicine and the Yale Cancer Center, recently shared his insights on a groundbreaking study titled “Evaluating Clinical Outcomes and the Role of Neoadjuvant Chemotherapy in Plasmacytoid Urothelial Carcinoma.” This significant research was revealed at the Society of Urologic Oncology’s 25th Annual Meeting in Dallas, Texas.
What is Plasmacytoid Urothelial Carcinoma?
Plasmacytoid urothelial carcinoma is a rare and aggressive subtype of bladder cancer, accounting for less than 5% of all urothelial cancers. This rarity poses considerable challenges for researchers, making it tough to gather comprehensive clinical data. Moreover, patients diagnosed with this variant face particularly poor outcomes, as existing staging methods often fail to accurately reflect the disease's true extent prior to treatment.
Key Findings and Challenges
Dr. Ghali highlighted that prior studies have relied heavily on institutional series, which offer limited scope. By utilizing the National Cancer Database, his team aimed to broaden the understanding of treatment outcomes and strategies utilized across various healthcare settings.
Key findings revealed that approximately 123 cases of plasmacytoid carcinoma were documented in the National Cancer Database, and with the addition of their own patient cohort, the total rose to just under 150. Unfortunately, these numbers are still relatively small, underscoring the need for further research.
From their analysis, it became evident that plasmacytoid urothelial carcinoma is associated with an alarming median survival rate of just 2 to 3 years. In a striking observation, the research discovered that clinical staging often underestimated the actual extent of the disease, particularly regarding lymph node involvement. Clinical assessments indicated that only around 8-9% of patients had nodal involvement before surgery, while pathological evaluations during radical cystectomy revealed that this figure escalated to between 25-30%.
The Role of Neoadjuvant Chemotherapy
The study also probed the effectiveness of neoadjuvant chemotherapy for this rare subtype. Ghali noted that although academic settings confidently prescribed chemotherapy prior to surgery for 65-75% of patients, the broader community practice reported a starkly lower rate of around 21%. Despite the frequent use of chemotherapy, statistical analysis did not conclusively support its role in improving overall survival outcomes. “There is a possibility that patients receiving chemotherapy are inherently healthier or younger, which may skew our understanding of the relationship between neoadjuvant therapy and survival rates," Ghali concluded.
Implications for Clinical Practice
Dr. Ghali emphasized the need for cautious interpretation of the findings, stressing that these results were primarily hypothesis-generating. "We urgently require high-quality, prospective studies to uncover the truth about treatment efficacy, particularly given the aggressive nature of this cancer."
A critical observation from the findings is the unique propensity of plasmacytoid cancers to metastasize peritoneally, as noted in a significant 78% of cases at Yale. This suggests a need for heightened vigilance in staging and treatment strategies for patients with this aggressive cancer.
Future Directions in Research
The future looks hopeful as new immunotherapies and targeted agents continue to emerge on the treatment horizon. Dr. Ghali’s team, along with others, is focusing on the development of strong translational models for these variant subtypes. Investigations into the potential role of new treatment methodologies, such as hyperthermic intraperitoneal chemotherapy (HIPEC) or intraperitoneal immunotherapy specifically targeting the abdominal metastasis, are concepts worth exploring for improved patient outcomes.
The pressing question remains: can research collaborations bolster our understanding and treatment of this challenging variant? Together, experts worldwide must combine their forces to tackle the clinical realities faced by patients suffering from plasmacytoid urothelial carcinoma.
Call to Action
As we continue to unearth the intricacies of this rare cancer, there is an urgent need to propel research initiatives forward and innovate treatment modalities. With a collective effort, we can pave the way for breakthroughs that this patient population desperately needs. The time to act is now—let’s not leave these patients behind.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)