Unveiling the Shocking Inequities in Access to Semaglutide: How Employment and Insurance Shape Your Chances!
2025-01-22
Author: Li
Introduction
In recent years, semaglutide—originally developed to manage diabetes—has transformed into a sensation for weight loss since its FDA approval in 2021. Its recognition skyrocketed, especially with celebrities publicly championing the drug. As of 2023, the introduction of tirzepatide, an even more potent medication, has only intensified this trend.
Disparities in Access
However, a deep dive into the healthcare system reveals a troubling truth: not everyone who could benefit from these groundbreaking anti-obesity medications has equal access to them. A newly published study from Boston University School of Public Health (BUSPH) has uncovered alarming disparities, highlighting that your type of insurance and employment status may significantly impact your likelihood of receiving semaglutide.
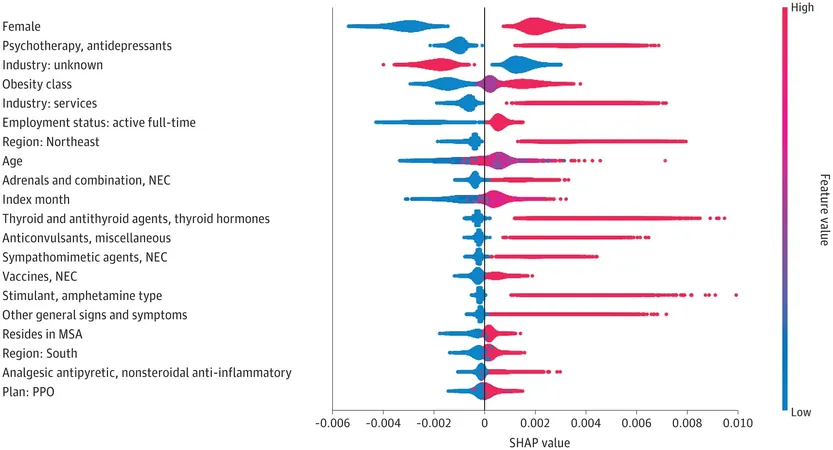
According to the study featured in JAMA Network Open, prescription rates varied dramatically based on factors such as insurance type, job industry, sex, and concurrent medication usage. For example, commercially insured, non-diabetic individuals with obesity, particularly women who had preferred insurance plans and were taking medications for conditions such as depression or hormonal imbalances, were more likely to receive this treatment. Conversely, males or those with less flexible insurance plans were at a disadvantage.
Employment and Insurance Influence
Professionals in high-paying sectors like finance and real estate also experienced higher rates of semaglutide prescriptions compared to their counterparts in retail jobs. This disproportionate access shines a light on the structural barriers faced by many individuals struggling with obesity—a health issue that is often simplistically blamed on lifestyle rather than treated as a standalone disease requiring medical intervention.
Changing Perspectives
As Andrew Stokes, an associate professor at BUSPH and the study's senior author, notes, the traditional approach to treating obesity often involved recommending lifestyle changes first, with medication only introduced once patients developed further health complications. However, emerging evidence suggests a significant necessity to change this paradigm, as achieving lifestyle change can be challenging due to biological resistance and external systemic barriers.
Insurance Coverage Gaps
The grim reality is that only one in four employers currently offer insurance that covers GLP-1 pharmaceuticals like semaglutide for weight management, while coverage is near universal for diabetes treatments. This inconsistency disproportionately affects those in lower-paying jobs or less beneficial insurance plans, exacerbating health inequalities.
Call for Policy Change
The research team hopes that their findings will prompt healthcare providers to better identify patients facing significant barriers to obesity treatment. They stress that understanding these disparities can lead to more informed policy changes that expand insurance coverage across various demographics.
Rethinking Obesity
Yet, the path forward is not just about policy. It also involves rethinking how we approach obesity itself. As Katherine Hempstead from the Robert Wood Johnson Foundation points out, existing barriers reflect deep-rooted health inequities in our system. Comprehensive studies are needed to fully understand the nature and size of these gaps.
Geographic Disparities
Notably, the study revealed that individuals living in the northeastern United States had higher rates of semaglutide utilization. Interestingly, patients with a Body Mass Index (BMI) of 40 or higher were more likely to begin treatment, suggesting a disturbing trend where physicians may reserve GLP-1 drugs solely for those with higher obesity levels, ignoring the FDA’s approval criteria for lower BMI thresholds.
Future Research Directions
The BUSPH team plans to continue their examination of inequities in GLP-1 access, potentially exploring connections with socioeconomic status, race, ethnicity, as well as Medicare and Medicaid coverage disparities. Currently, Medicare restricts GLP-1 drug coverage to diabetic patients, while Medicaid’s provisions vary significantly by state.
Conclusion
As discussions around obesity treatments and the healthcare landscape heat up, the future of access to semaglutide remains uncertain, especially in the political sphere. With continued debates over health policy, the essential question remains: will the next administration recognize and rectify these significant barriers to care? It's clear that the fight against obesity is not just about the medications available; it's about ensuring equitable access for all individuals in need. As the clock ticks, the call for change echoes louder than ever.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)