Unveiling the Link Between Personality Disorders and Depression Progression: A Groundbreaking Study
2025-06-02
Author: Yu
Understanding Unipolar Depression (UD) and its Complexities
Unipolar depression (UD), a widespread psychiatric condition, manifests through relentless feelings of sadness, hopelessness, and a disconnection from activities once enjoyed. Accompanying symptoms often include changes in energy, sleep disturbances, appetite shifts, dwindling focus, and even suicidal thoughts. The intricate nature of UD stems from a blend of biological, psychological, and social factors, making it a significant concern for global public health.
The Interplay of Personality Disorders (PD) and Depression
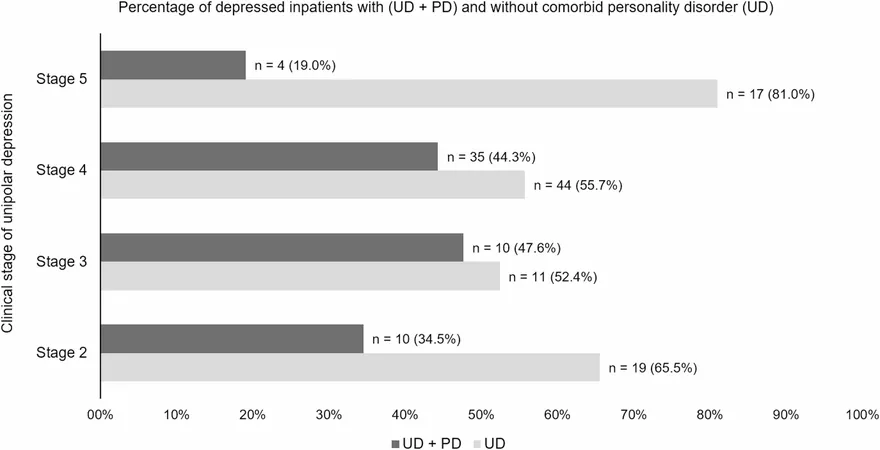
Similar to UD, personality disorders (PD) are prevalent psychiatric issues that present a myriad of challenges, from poor health outcomes to increased unemployment and reduced life expectancy. Marked by a pervasive pattern of maladaptive traits and behaviors emerging in early adulthood, PD can lead to significant personal distress and impaired functioning. Alarmingly, studies indicate that 40-50% of inpatients with UD also grapple with a comorbid PD, which correlates with graver UD outcomes, higher rates of treatment resistance, and persistent depressive symptoms.
Evaluating Depression Progression: A Clinical Staging Model
To better understand the progression of UD, a clinical staging model was introduced, updated over the years to classify UD into five stages, ranging from prodromal symptoms to chronic episodes lasting over two years. This tool not only clarifies the state of the illness but also aids in treatment selection and assessing therapeutic effectiveness.
The Critical Role of Social Support in Mental Health
The significance of social factors in mental health care is steadily gaining recognition. Social support (SS) reflects an individual’s perception of the assistance available from relationships and networks, especially in times of stress. Research has shown that patients with UD who report low levels of SS face worse outcomes, emphasizing SS as a potential protective factor against depressive symptoms.
Groundbreaking Research Objectives and Findings
This innovative study set out to explore several crucial objectives, including the prevalence of PD among inpatients diagnosed with UD and the SS levels between groups with and without comorbid PD. Conducted with a sample of 150 inpatients at a leading university hospital in Brazil, results indicated that those with comorbid PD reported significantly lower SS levels, complicating their recovery.
Implications of the Study's Findings
The research highlights a concerning trend: reduced SS complicates the recovery process for patients with UD, particularly those also battling PD. It underscores the importance of psychosocial interventions aimed at enhancing social and interpersonal functioning, which could lead to better treatment outcomes.
Moving Forward: Recommendations for Future Research
Acknowledging the study's limitations, including the focus solely on inpatients with UD, it paves the way for further research, especially among outpatient populations. The findings advocate for greater attention to social determinants of mental health and suggest that effective management of comorbid PD in UD patients could ultimately reduce hospital admissions.
Conclusion: A Call to Action
The alarming connection between personality disorders and depression progression demands immediate attention in psychiatric treatment approaches. By enhancing support systems and focusing on the social aspects of mental health, we may better equip patients on their journey to recovery, ultimately improving their quality of life.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)