Unveiling the Hidden Dangers of Stress Hyperglycemia: How Your Blood Sugar Levels Could Determine Your Surgical Success!
2024-11-02
Author: Yu
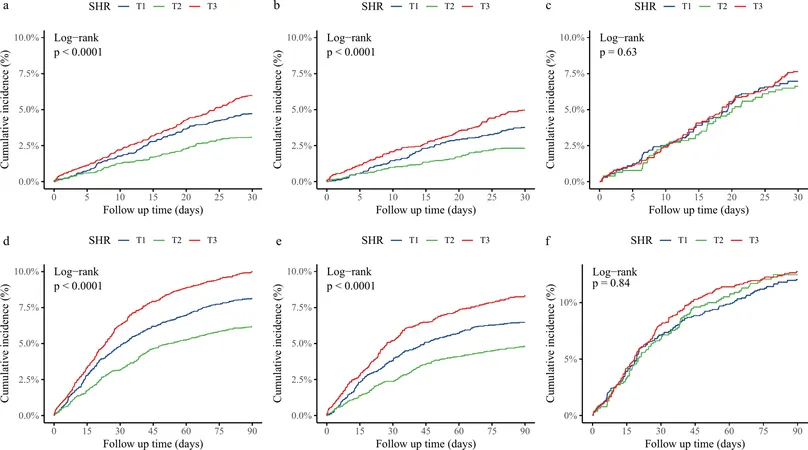
In an extensive study analyzing over 12,000 surgical patients, researchers have unveiled significant connections between stress hyperglycemia ratio (SHR) and the likelihood of experiencing major adverse cardiovascular and cerebrovascular events (MACCE) following noncardiac surgeries (NCS). Conducted at Seoul National University Hospital, this research sheds crucial light on preoperative blood glucose levels and their implications for surgical outcomes.
Study Overview and Cohort
The study is part of the INSPIRE medical research database, encompassing a staggering 274,919 patients who underwent various surgical procedures from January 2011 to December 2020. After refining the cohort based on age and medical history, researchers examined 12,899 surgical patients. The cohort was predominantly older adults, with 86% aged 45 or over and a significant representation of females (51%) compared to males (49%).
Significant Findings on SHR and Postoperative Risk
The findings reveal that both the lowest and highest SHR groups bore increased risks for MACCE—by 35% and 34% respectively—within 30 days post-surgery. Notably, patients in the highest SHR tertile who did not have diabetes faced a staggering 60% increased risk of complications in the same timeframe. On the flip side, non-diabetic patients also exhibited a concerning U-shaped relationship between SHR and MACCE, reinforcing the need for meticulous blood sugar management.
Blood Glucose Levels: A Double-Edged Sword?
While stress-induced hyperglycemia is often seen as a natural response to surgical stress, this study indicates that unmonitored spikes in blood glucose could lead to dire outcomes. What is particularly alarming is that some patients experiencing stress hyperglycemia may actually be undiagnosed diabetics, further complicating preoperative assessments.
Implications for Surgical Practices
Health professionals from various fields—surgeons, cardiologists, and anesthesiologists—are now urged to measure blood glucose and glycated hemoglobin levels preoperatively. By calculating the SHR, healthcare providers can better estimate risks for MACCE in patients, especially those without a diabetes diagnosis. This could lead to improvements in postoperative care and recovery, emphasizing a proactive approach to managing blood sugar levels.
Cautionary Notes on the Study
Despite its ambitious scope, the study calls for caution. Conducted in a single institution primarily comprising Asian patients, the results may not extrapolate universally. Additionally, the observational nature of the study may harbor confounding variables that were not accounted for, which could influence the outcomes.
Conclusion: Charting a Path Forward
As the medical community discerns the relationship between stress hyperglycemia and surgical outcomes, it becomes evident that paying close attention to preoperative blood sugar levels is critical. This research not only signifies a pioneering evaluation of SHR's impact on postoperative risk but also advocates for routine screenings of blood glucose in surgical candidates. Setting aside just a few moments to monitor and control blood sugar could mean the difference between a smooth recovery and serious complications.
As we march forward, let’s ensure that controlling blood glucose is not merely an afterthought for surgical patients but a leading part of preoperative care!
Don't Take Your Health for Granted!
If you or someone you know is preparing for surgery, now is the time to talk to your doctor about blood sugar management strategies. Your life could depend on it!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)