Unmasking COVID-19: How Population-Specific Factors Shape Infection Risk and Severity in Israel
2025-08-04
Author: Daniel
The Global Threat of Acute Respiratory Infections
Acute respiratory tract infections (ARI) remain a colossal public health challenge, accounting for millions of deaths annually, particularly affecting the young, elderly, and immunocompromised. These infections, caused by various RNA viruses—including coronaviruses—span symptoms from mild colds to severe respiratory distress.
The COVID-19 Pandemic: A Stark Reality
Since its emergence in late 2019, COVID-19, triggered by the SARS-CoV-2 virus, has infected over 700 million globally and claimed more than 7 million lives. In Israel alone, SARS-CoV-2 cases reached nearly 4.9 million, with significant mortality recorded.
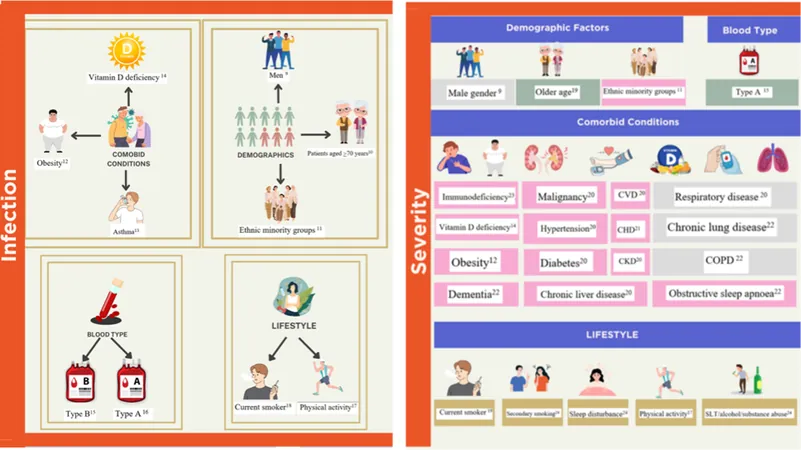
The clinical spectrum of COVID-19 varies widely, with some individuals asymptomatic while others face dire respiratory conditions. Multiple epidemiological risk factors contribute to this landscape, yet individual susceptibility remains enigmatic, with some unexplainably developing severe disease despite lacking known risk factors.
Diving into Diversity: The Israeli Context
Israel, home to approximately 9.9 million people, showcases a rich tapestry of ethnicities and cultures, most prominently Jewish and Arab communities. Each group has distinct healthcare-seeking behaviors and societal factors that likely influence COVID-19 susceptibility and outcomes.
Understanding the intricate web of factors that affect COVID-19 within these population segments is crucial for devising effective public health strategies. This study aims to highlight the epidemiological risk factors affecting the Israeli population and compare them with findings from other regions.
Weighing the Evidence: Study Design and Methodology
This study surveyed adults in Israel who underwent SARS-CoV-2 testing between July 2021 and August 2022. Participants were recruited via SMS links to online surveys, allowing responses in Hebrew, Arabic, Russian, and English, ensuring wide accessibility.
Data included demographic details, health status, and COVID-19 episodes, capturing a robust picture of the factors influencing infection and severity.
Key Findings: Risk Factors for Infection and Severity
Analysis revealed that various factors—including age, gender, ethnicity, education level, BMI, and vaccination status—significantly influenced COVID-19 outcomes. The study found an increased susceptibility among Arab populations compared to the Jewish majority, echoing trends seen in other minority groups globally.
Vaccination demonstrated a profound protective effect, drastically reducing the odds of infection and hospitalization. However, the emergence of the Omicron variant highlighted a decline in vaccine effectiveness, particularly among those infected after January 1, 2022.
The Importance of Education and Socioeconomic Status
Higher education levels correlated with lower infection and hospitalization rates, suggesting that education impacts health literacy and access to care. This finding aligns with global observations that socio-economic disparities significantly shape health outcomes during the pandemic.
Challenges and Limitations: A Collaborative Call for Further Research
While the study reveals critical insights, limitations such as potential biases in self-reported data and regional selection effects must be acknowledged. A broader approach involving diverse population segments is essential for a more granular understanding of COVID-19 susceptibility and severity.
Conclusion: Preparing for Future Pandemics
Identifying population-specific risk factors is vital to enhancing pandemic readiness. This research offers a framework that integrates genetic and epidemiological data, paving the way for targeted strategies to mitigate future outbreaks in Israel and beyond. As the world navigates the evolving threat of respiratory infections, understanding the nuances of population dynamics will be key in safeguarding public health.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)