Uncovering the Deadly Impact of Pneumococcal Pneumonia in Adults and Seniors: A Comprehensive Review of Serotype Distribution
2025-03-29
Author: Daniel
Community-acquired pneumonia (CAP) remains a formidable health challenge worldwide, particularly affecting the very young and the elderly. With a staggering 2.6 million deaths attributed to lower respiratory infections globally in 2019, CAP ranks as the fourth leading cause of mortality (World Health Organization). Among the chief culprits is *Streptococcus pneumoniae* (S. pneumoniae), known to be the predominant bacterium responsible for these infections, with its virulence outpacing other pathogens combined.
Over 90 serotypes of *S. pneumoniae* have been identified, yet a mere subset—about 10 serotypes—accounts for approximately 62% of invasive pneumococcal disease (IPD) cases worldwide. This variance in serotype prevalence can depend on factors like geographical location and population demographics. Alarmingly, the majority of pneumonia-related deaths can be prevented through vaccination.
For the elderly, two main types of pneumococcal vaccines are available: the pneumococcal polysaccharide-based vaccine (PPSV23) and pneumococcal conjugate vaccines (PCVs). The PPSV23, approved in 1983, targets 23 serotypes responsible for 60-76% of invasive disease but has limited effectiveness among infants and seniors, who often do not mount adequate immunogenic responses.
In response to these limitations, pneumococcal conjugate vaccines, like the original 7-valent (PCV7) vaccine introduced in 2000, were developed. Notably, following its adoption in the U.S., a remarkable 76% decrease in IPD among vaccinated children was observed. However, this victory came with a cautionary note as non-vaccine serotypes increased by 22%, particularly serotype 19A.
In subsequent years, PCV10 and PCV13 were introduced, increasing the serotype coverage and enhancing protection among older adults, with studies indicating that approximately 20%-25% of IPD cases in seniors could potentially be prevented with these vaccines. The Advisory Committee on Immunization Practices (ACIP) in the U.S. now recommends administering PCV13 along with PPSV23 for individuals over 65.
More recently, the introduction of PCV15 and PCV20 in 2021 has further expanded options for adults at risk of serious pneumococcal disease. However, vaccination coverage rates among older adults remain relatively low, raising concerns about the effectiveness of these programs in continents like Europe and the Americas.
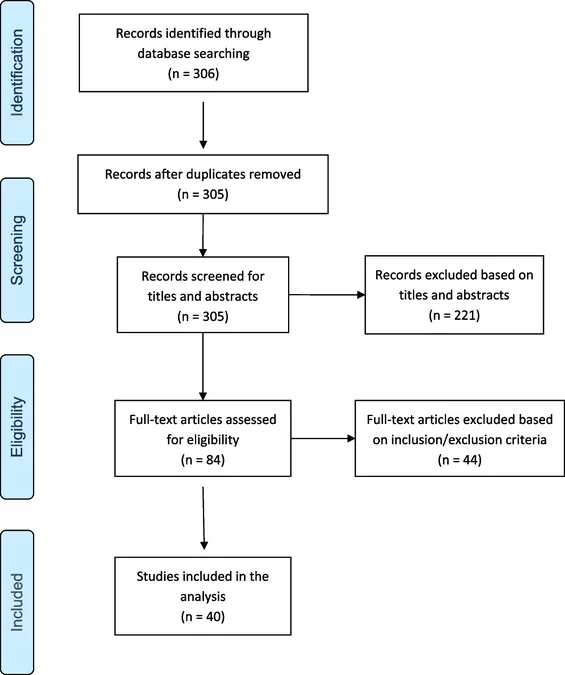
A systematic review involving 40 studies conducted across 18 countries reveals compelling data about the serotype distribution and burden of pneumococcal pneumonia among adults and the elderly. This review highlights that serotype 3 consistently topped the list as the most prevalent serotype causing CAP, followed by serotypes 1, 14, 7F, and 19A. Striking disparities exist in serotype prevalence based on geographic regions, illustrating the need for localized vaccination strategies.
A troubling trend is the rising incidence of non-vaccine serotypes post-PCV introduction, suggesting that while current vaccines are vital, they must continually adapt to effectively combat emerging threats. For instance, serotype 15A emerged as the leading non-vaccine type, reinforcing the need for vigilant monitoring and potential updates to vaccine formulations.
To address these dynamically shifting epidemiologies, there is an urgent call for new vaccines that consider not just changing serotypes but also local epidemiological data and health burdens. The evidence presented in this review underscores the necessity for robust vaccination programs, particularly targeting vulnerable populations, and the significance of ongoing research into the impact of new vaccine introductions.
As pneumonia remains a leading cause of mortality, urgent action to optimize vaccination strategies is essential to fulfill the promise of prevention, especially among seniors whose immune systems are already compromised by age and chronic diseases. Monitoring serotype trends and fostering public health initiatives will be pivotal to mitigating the impact of pneumococcal pneumonia as we navigate through an evolving healthcare landscape.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)