Uncovering Extrapulmonary Tuberculosis in Khuzestan, Iran: A Comprehensive Study from 2002 to 2023
2024-12-25
Author: Wei Ling
Introduction
Tuberculosis (TB) remains a leading cause of mortality globally, with extrapulmonary tuberculosis (EPTB) being a significant but often overlooked variant. Between 2002 and 2023, Khuzestan province in southwest Iran has been the focus of an extensive study aiming to shed light on the prevalence of EPTB among patients, whether they also had pulmonary TB (PTB) or not. This groundbreaking research fills a crucial gap in understanding TB's impact in this endemic region.
Research Methodology
This retrospective study utilized patient records from the Tuberculosis Regional Reference Laboratory in Khuzestan. Researchers meticulously analyzed data spanning nearly two decades, covering confirmed cases of both EPTB and combined EPTB with PTB. The study rigorously excluded records with incomplete information or military-associated TB cases. Key information such as age, gender, affected organs, and residential location were collected to form a comprehensive epidemiological profile.
Key Findings
The analysis revealed an eye-opening statistic: a total of 12,900 EPTB-related medical records, with 12,836 meeting the study's criteria. This included 5,991 patients suffering from both PTB and EPTB, alongside 6,845 individuals who had EPTB exclusively. The average age of male patients with EPTB was significantly higher than their female counterparts—37.5 years compared to just 31.2 years. This difference raises questions about gender-related vulnerabilities and immune response.
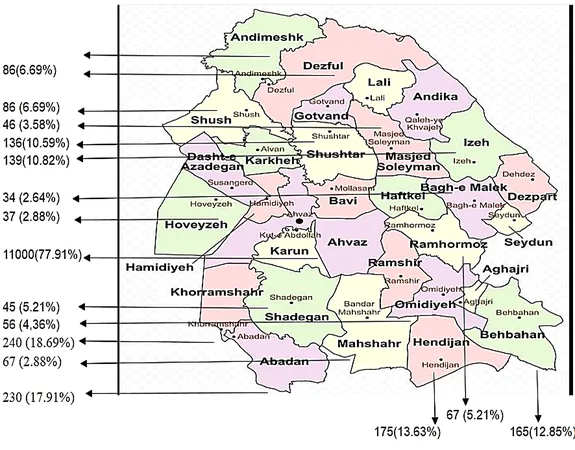
The study's geographical scope also unveiled enlightening trends. The majority of EPTB cases originated from various cities in Khuzestan, with a notable concentration in Ahvaz. Concerningly, a significant portion of both EPTB and PTB patients were found to be HIV positive, highlighting a troubling intersection between these two health crises.
Discussion: The Broader Implications of EPTB Findings
Understanding EPTB is crucial for healthcare providers, especially since this form of TB can lead to serious conditions such as meningitis or renal impairment. With 21% of AIDS patients also suffering from EPTB, the urgency for improved diagnostic practices cannot be overstated. The implications of these findings extend beyond Khuzestan; as observed globally, the prevalence of EPTB holds pivotal consequences for public health strategies.
In line with previous studies, lymphadenitis was identified as the most common manifestation of EPTB in this region, accounting for approximately 44.19% of cases. Recognizing the clinical manifestations of TB allows for swift intervention, which is critical given that advanced TB can lead to severe morbidity or mortality if left untreated.
Conclusion and Future Directions
The substantial findings from this study underscore the need to enhance awareness and diagnostic capabilities regarding EPTB in Iran and other endemic regions. The researchers emphasize the unique epidemiological patterns revealed through this analysis, advocating for targeted interventions that reflect the demographic nuances of TB in Khuzestan. The lessons learned here could serve as a guide for future research and policy formulations, aiming for a future where TB, including its extrapulmonary forms, is effectively controlled and ultimately eradicated.
As TB continues to pose a severe threat to public health, comprehensive studies like this one are vital in paving the way for informed healthcare policies and practices. The fight against tuberculosis must be reenergized, with a focus on both prevention and the eradication of its various strains.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)