The Surprising Truth: Fat Mass is a Stronger Indicator of Survival in African Children with Severe Pneumonia than Muscle Mass!
2024-09-30
Introduction
Pneumonia is a leading killer of children under five, contributing to a staggering 14% of mortality in this age group. Alarmingly, children suffering from severe pneumonia and poor nutritional status face even graver risks of mortality. While medical professionals have relied on traditional anthropometric measurements to assess children’s nutritional status, recent findings suggest that understanding body composition—specifically fat and muscle mass—may be crucial in predicting outcomes.
Study Objectives
In a groundbreaking study from Uganda and Kenya, researchers set out to determine whether fat mass serves as a better predictor of six-month survival compared to muscle mass in children aged 6 to 59 months hospitalized with severe pneumonia. The study, part of the COAST-Nutrition trial, explores this pivotal question, potentially changing how health professionals approach nutritional assessments in such vulnerable populations.
Methodology
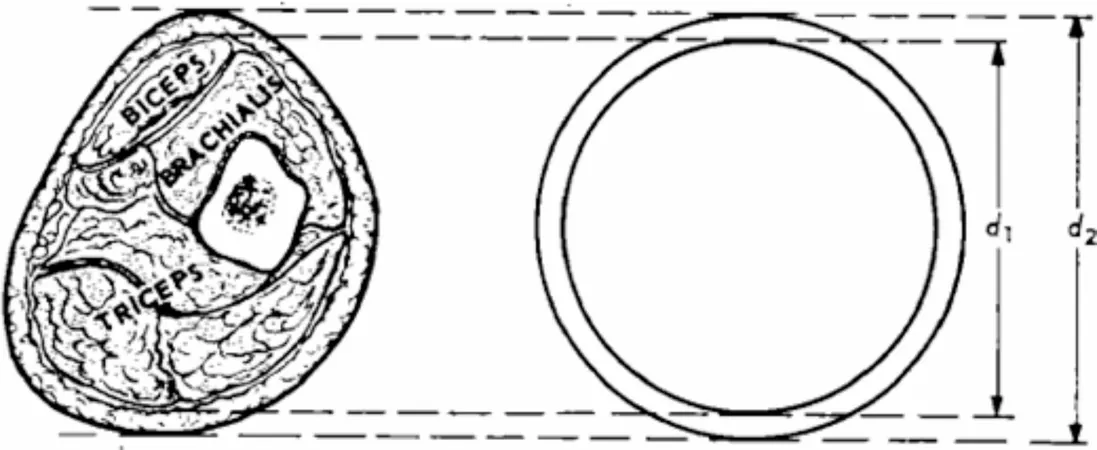
The prospective cohort study included 369 children, predominantly male with a median age of 15 months. The children were assessed for weight, height, mid-upper arm circumference (MUAC), arm-fat-area (AFA), arm-muscle-area (AMA), and arm-muscle-circumference (AMC). The analysis looked at how these indices correlated with survival over a follow-up period of six months.
Researchers utilized Receiver Operator Characteristic (ROC) curves to compare the efficacy of fat versus muscle mass indices in predicting survival outcomes. A total of 16 participants (4.3%) succumbed during the study, highlighting the severe impact of this condition.
Key Findings
The study's results indicated that while the AFA was slightly more predictive of survival than arm muscle indices, no significant statistical difference was observed (AUC 0.75 for AFA vs. 0.61 for AMA and 0.63 for AMC). Notably, both AFA and MUAC provided comparable predictions for survival. Additionally, increases in AFA and AMC significantly improved survival rates, suggesting their importance in clinical assessments.
These findings align with the physiological understanding that during illness, particularly in catabolic states like pneumonia, the body utilizes fat stores to protect protein reserves essential for immune function. Higher fat mass not only provides energy but also supports overall immune health, indicating a complex interplay between body composition and recovery.
Implications for Child Health
The study underscores the importance of reevaluating traditional nutritional assessments and highlights the need for innovative interventions that could improve survival rates. The recommendation is clear: fat mass should be prioritized in assessments of severely ill children.
This is particularly crucial when considering nutritional supplementation for children recovering from pneumonia. As the study suggests, emphasizing fat mass could lead to tailored interventions that significantly enhance survival outcomes, thus reshaping public health strategies in pediatric healthcare.
Conclusion
The results of this study challenge long-held beliefs regarding the significance of muscle mass in the prognosis of severe pneumonia among children. Ultimately, the evidence suggests that targeting fat mass could be key to improving survival rates, offering a new perspective in managing and treating hospitalized children facing life-threatening conditions.
As pneumonia continues to claim young lives in Africa, understanding these insights could pave the way for preventive and therapeutic measures, ultimately saving more children and giving them a fighting chance against this deadly infection.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)