The Surprising Connection: How Autoimmune Diseases may Lead to Schizophrenia and Vice Versa!
2024-11-16
Author: Siti
Introduction
Schizophrenia (SCZ) is a debilitating neuropsychiatric disorder recognized for its profound impact on individuals and society as a whole. With an estimated global prevalence of approximately 1%, SCZ is one of the top ten causes of serious illness worldwide. Alarmingly, individuals diagnosed with SCZ may live around 14.5 years less than the general population, highlighting the severe ramifications on public health and the economy. In the United States alone, the financial costs associated with SCZ soared to nearly $343.2 billion in 2019, surpassing previous figures from 2013.
Understanding the Link Between Autoimmune Diseases and Schizophrenia
The development of SCZ is a complex interplay of genetic and environmental factors, yet its precise causes remain elusive. Recent research has increasingly pointed to a potential link between immune system dysregulation, autoimmunity, and SCZ. The hypothesis suggests that autoimmune diseases may not only increase the likelihood of developing SCZ but that existing SCZ might also heighten the risk of subsequent autoimmune conditions.
Historical Context and Mixed Findings
Historically, studies investigating these connections have yielded mixed results. Some literature supports a heightened risk of SCZ in patients with diseases like systemic lupus erythematosus (SLE), while others indicate a protective effect from conditions like ankylosing spondylitis (AS). Notably, certain autoimmune conditions show varied relationships with SCZ; for instance, inflammatory bowel disease (IBD) and type 1 diabetes have been associated with an increased risk of developing SCZ.
Groundbreaking Study: Methods and Findings
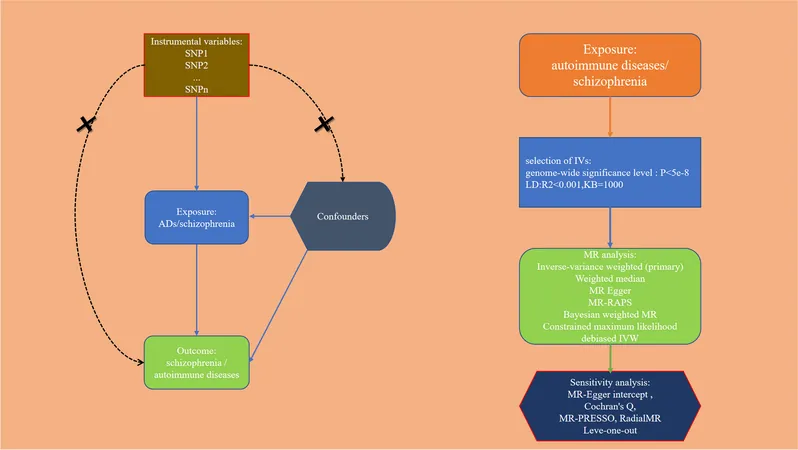
In a groundbreaking study utilizing bidirectional Mendelian randomization (MR), researchers sought to clarify these complex associations. By analyzing genetic variations known to influence both autoimmune diseases and SCZ, the study aimed to unveil whether one condition causally affects the other.
The study focused on European populations and employed rigorous statistical techniques to ensure robust conclusions. Researchers meticulously selected single nucleotide polymorphisms (SNPs) as instrumental variables (IVs) to meet the stringent criteria necessary for MR analysis. These analyses rectified previous observational biases, aiming for clarity in the causal connections between autoimmune diseases and SCZ.
Investigating the Results
Results revealed intriguing findings: AS was found to correlate with an increased risk of SCZ, countering earlier studies suggesting the opposite. Surprisingly, conditions like celiac disease (CeD) and type 1 diabetes demonstrated an association with a reduced risk of developing SCZ, aligning with some cohort studies while contradicting others. For diseases such as multiple sclerosis (MS), psoriasis (PsO), rheumatoid arthritis (RA), and IBD, further links emerged, suggesting that individuals with SCZ evidently faced higher risks of these autoimmune conditions.
Implications for Future Research and Clinical Practice
The insights gained are pivotal for both researchers and clinicians. The findings compel a reassessment of historical perspectives about the relationship between SCZ and autoimmune diseases, emphasizing the need for ongoing investigations to unveil underlying immunological mechanisms. Understanding this dynamic interaction holds the potential for novel therapeutic strategies that address both psychiatric and autoimmune concerns.
Conclusion
As research evolves, it becomes apparent that more comprehensive analyses across diverse populations are essential. The current study, while groundbreaking in its methodology, also calls for caution. With limited focus on European-descent populations, its findings may not translate universally. Ultimately, these revelations underscore a crucial moment in psychobiological research—prompting a holistic approach wherein patients with mental health conditions like SCZ are routinely evaluated for autoimmune disorders, thus paving the way for improved diagnoses, interventions, and patient outcomes.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)