The Shocking Truth Behind Basal Cell Carcinoma's Low Immunogenicity: New Research Unveils Key Factors
2025-04-22
Author: Yu
Understanding Basal Cell Carcinoma's Battle Against the Immune System
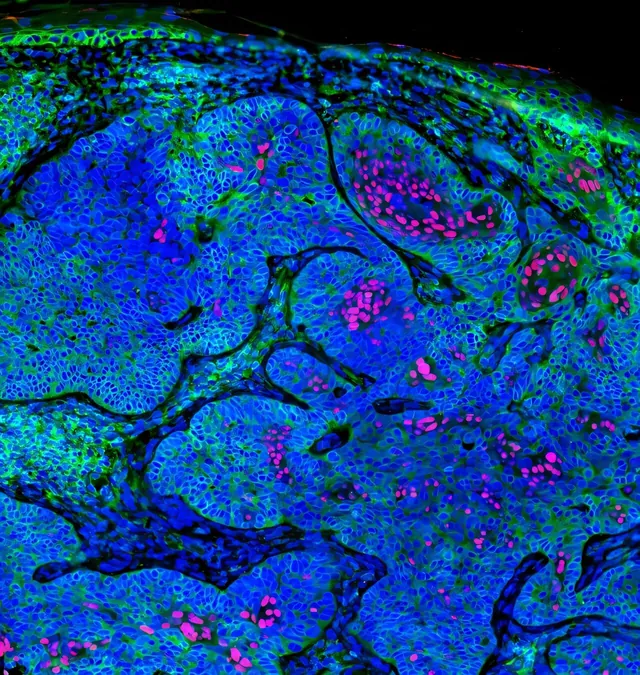
Basal cell carcinoma (BCC) emerges as the most common form of skin cancer, surprisingly harboring the highest tumor mutational burden. Yet, it shocks researchers with its low immunogenicity, making it laidback against immune therapies that often work wonders for other cancers.
The Science of Immune Evasion
At the heart of this challenge lies compromised antigen presentation—one of the top mechanisms that hamper a cancer's ability to be recognized and attacked by the immune system. In particular, a lack of human leukocyte antigens class I (HLA-I) components is alarmingly prevalent in these immune-excluded cancers.
Antigen presentation, crucial for prompting CD8+ T cells to attack cancer cells, is systematically undermined by BCCs, displaying a sophisticated evasion strategy that hinders immune recognition.
Revolutionary Research Insights
A compelling new study led by Dr. Shawn Demehri, a physician-investigator at Massachusetts General Hospital and Harvard Medical School, reveals groundbreaking insights into this phenomenon published in the journal Cell Reports. His team scrutinized a significant collection of primary human BCCs, comparing them with squamous cell carcinomas (SCCs), which have shown better response to immune therapies.
The findings were striking: primary BCCs exhibited an immune-excluded phenotype, marked by minimal HLA-I expression, even in their early development stages.
The Cell of Origin Holds the Key
One of the most shocking revelations is that BCC's low immunogenicity ties back to a stem-like quiescent program derived from its cell of origin, which actively suppresses antigen presentation mechanisms. Interestingly, reversing this suppression holds the potential to boost BCC’s responsiveness to immunotherapy.
Clinical Implications and Future Trials
Dr. Demehri passionately advocates for innovative treatment strategies, revealing that topical entinostat can increase antigen presentation in BCC models. This treatment combined with FDA-approved topical immunotherapy, imiquimod, demonstrated high efficacy in blocking BCC growth and shows promise for enhancing immune activation.
Such findings hint at the dawn of a new era in BCC treatment, suggesting a first-in-human clinical trial to evaluate the effectiveness of this combination therapy. The implications for better treatment strategies shine bright on the horizon, offering new hope for patients fighting against this silent yet prevalent foe.
The Bigger Picture: SCC vs. BCC
While SCCs show a staggering 49.3% objective response rate to PD-1 therapy, metastatic BCCs lag behind with only a 21% response rate. Intriguingly, organ transplant recipients on immunosuppressants face a substantially higher risk of developing SCCs, yet only a modestly increased risk for BCC, reinforcing the notion that BCC’s intrinsic immunogenic barriers need to be addressed.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)