The Hidden Struggles: A Closer Look at Obsessive-Compulsive Symptoms in Schizophrenia Patients on Clozapine
2025-01-23
Author: Mei
Schizophrenia: A Multifaceted Disorder
Schizophrenia—a multifaceted mental health disorder—causes varied symptoms in affected individuals, ranging from hallucinations to cognitive impairments. This disorder manifests differently for each person; some may experience intense episodes of positive symptoms, while others may struggle with negative symptoms like social withdrawal or emotional flatness.
Understanding the Treatment Landscape
The treatment of schizophrenia primarily revolves around pharmacological methods, utilizing antipsychotic medications, alongside non-pharmacological strategies that focus on enhancing social and occupational functioning. Physicians often weigh a patient's specific clinical presentation when deciding between typical (first-generation) and atypical antipsychotic medications, as current studies indicate limited efficacy disparity between these classes.
Among the medications available, clozapine stands out for treating treatment-resistant schizophrenia (TRS), a condition where positive symptoms persist despite the administration of at least two antipsychotic medications. It affects around 20-25% of patients, posing significant challenges in managing schizophrenia effectively.
An Overlap with Obsessive-Compulsive Symptoms
Obsessive-Compulsive Disorder (OCD) is marked by persistent, intrusive thoughts and repetitive behaviors. Patients with OCD experience considerable distress, which significantly impairs daily life. Interestingly, patients with schizophrenia can also exhibit obsessive-compulsive symptoms (OCS), either alongside or independently of a formal OCD diagnosis.
Research indicates that OCS may manifest at various points during a patient’s schizophrenia trajectory—before diagnosis, coinciding with psychotic episodes, or even as a reaction to treatment. Particularly alarming is the 38.9% rate of OCS development in patients treated with clozapine, starkly higher than those on other atypical antipsychotics.
The complexities surrounding clozapine are accentuated by its benefits and potential risks. Initially, clozapine raised safety concerns due to the risk of agranulocytosis—a severe drop in white blood cells—leading to its market withdrawal in the 1970s and subsequent restrictions on its use. The unique mechanism of clozapine, which includes potent antiserotonergic effects, may lead to the induction or exacerbation of OCS in some patients.
What's Behind the Numbers?
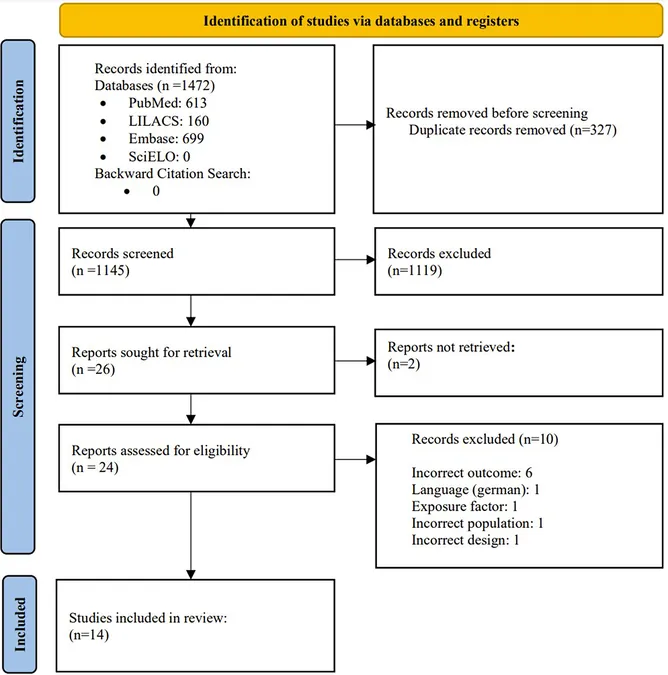
A systematic review revealed that the prevalence of OCS among clozapine-treated patients varies widely—from as low as 20% to a shocking 76%. Factors influencing this variability include differences in definitions and diagnostic assessments among studies, the inclusion of medications that may contribute to OCS, and other demographic variables impacting the overall findings.
Most concerning is the impact that OCS has on the overall quality of life and functioning of schizophrenia patients. The presence of OCS can lead to lowered mental wellbeing, complicating the treatment landscape for healthcare providers already challenged by the complex nature of schizophrenia.
The Need for Targeted Research
There is an urgent need for more in-depth studies to understand the intersection of clozapine treatment and OCS better. Current findings have opened avenues for investigation about whether the dosage of clozapine or the duration of treatment plays a pivotal role in OCS development.
The ongoing dialogue regarding the pharmacological versus therapeutic approaches to mitigating OCS brings up critical points—can adjunct therapies such as SSRIs provide relief? How much do individual factors like genetic predisposition and metabolic responses to clozapine contribute to the emergence of symptoms?
A Call for Clinical Awareness
In summary, mental health professionals must remain vigilant in monitoring patients on clozapine for any developing OCS. Understanding the prevalence and impact of these symptoms can drastically change the approach to treatment and ultimately improve the quality of life for patients struggling with both schizophrenia and OCD symptoms.
Statistical variability highlights the urgent necessity for standardized assessments and longitudinal studies, ensuring healthcare practitioners can fine-tune their treatment plans to address the full scope of their patients' needs. The road forward must prioritize patient-centered care, recognizing the unique challenges in managing the complex interplay between schizophrenia and OCS.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)