Surprising Findings in PD-1 Function Could Revolutionize Cancer Treatments: Are Current Models Misleading Us?
2025-01-08
Author: Ming
Recent research conducted at the University of California, San Diego (UCSD), has unveiled striking differences in the immune checkpoint protein PD-1 between humans and rodents. Published in Science Immunology, this study challenges decades of assumptions in immunology and may significantly influence the future of cancer therapy.
The Unexpected Discovery of the PEQ Motif
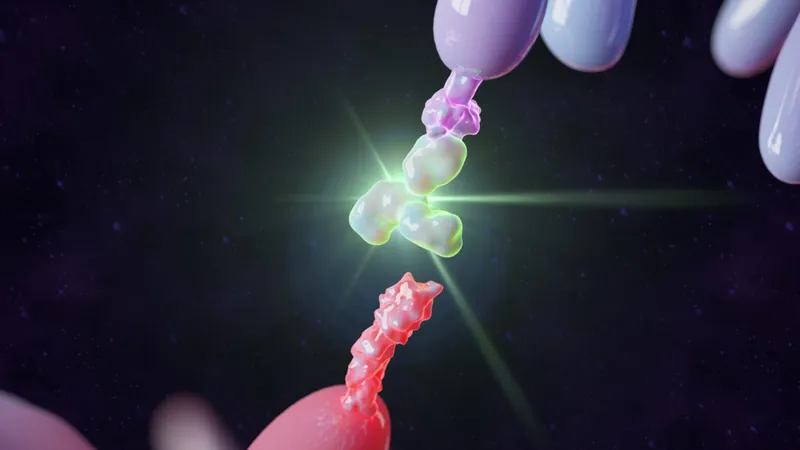
For a long time, scientists assumed that PD-1 in mice and humans was functionally identical due to the presence of conserved signaling features. However, lead researcher Enfu Hui, PhD, argues that this belief is fundamentally flawed. A key finding from this investigation is the identification of a specific three-amino-acid sequence known as the PEQ motif, which is present in human PD-1 but entirely missing from the rodent version. This motif plays a crucial role in stabilizing SHP-2, a phosphatase that is integral to PD-1’s ability to suppress T-cell activation.
The absence of the PEQ motif renders rodent PD-1 less efficient in binding SHP-2, leading to less effective T-cell suppression. This discrepancy may explain why certain PD-1-targeted therapies have shown limited success in human patients despite promising results in rodent models.
Insights from Evolution
Through phylogenetic analysis, the research team traced the divergence of PD-1 functionality back to the Cretaceous–Paleogene (K–Pg) boundary, around 66 million years ago, a time marked by widespread extinctions. Hui speculates that rodents are exceptions among vertebrates, which tend to retain the PEQ motif. Why rodents evolved to lose this sequence remains an intriguing question and may have connections to adaptive advantages during environmental changes and pathogen interactions.
The Impact on Humanized Models
To assess the functional implications of the PEQ motif, researchers engineered a "humanized" version of PD-1 in mice by swapping the intracellular domains of the mouse protein with those from humans. The results were remarkable: tumors developed significantly larger in these modified mice compared to those expressing native mouse PD-1. This reinforces the notion that human PD-1 possesses a stronger immunosuppressive capability, playing a vital role in tumor progression.
Dr. Takeya Masubuchi, the lead author of the study, emphasizes that relying on mouse PD-1 in current preclinical models may lead to an underestimation of the effectiveness of anti-PD-1 therapies. He advocates for reevaluating therapeutic strategies that consider quantitative differences in PD-1 functionality across species.
Redefining Preclinical Research
This research sheds light on the pressing need for more sophisticated models to study PD-1 and similar immune checkpoint proteins. Although rodents remain widely used in immunological research for their cost-effectiveness and availability, their evolutionary divergence from humans poses substantial limitations.
Masubuchi suggests a paradigm shift in research practices: "While humanized mouse models are useful, they might not completely bridge the existing gaps. It may be essential to explore alternatives like primate models or other mammalian species with PD-1 structures more akin to humans."
The study not only addresses PD-1 but also raises pertinent questions about the broader generalizability of rodent-based research findings. As Hui points out, significant molecular and cellular differences exist between mice and humans, particularly in immune system genes. This study meticulously demonstrates these discrepancies for PD-1, a critical target in the realm of cancer immunotherapy.
Transforming Cancer Immunotherapy
Identifying and addressing these functional differences can substantially enhance the predictive accuracy of preclinical models, which is crucial for designing effective dose-response studies and understanding the mechanisms of PD-1 inhibition.
"This research raises more questions than answers," Hui reflects, "and that’s the hallmark of meaningful science. It opens the door for collaboration and innovation in developing better models not only for PD-1 but also for other immune checkpoints."
Masubuchi underscores the urgency of this transition: "By recognizing current model limitations and striving for more accurate representations of human biology, we can significantly boost the development of life-saving therapies."
With these groundbreaking findings, the landscape for cancer treatment might be on the verge of transformation—ushering in an era where more precise models lead to better therapeutic outcomes for patients battling cancer.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)