Revolutionary Study: Is Microultrasonography the Future of Prostate Cancer Detection Over MRI?
2025-03-24
Author: Yu
Revolutionary Study on Microultrasonography and Prostate Cancer Detection
Exciting new research indicates that microultrasonography-guided biopsies could be just as effective as traditional MRI-guided biopsies in detecting clinically significant prostate cancer (csPCa) in biopsy-naïve men. This groundbreaking finding has emerged from a comprehensive international multicenter, phase 3 randomized study published in the esteemed Journal of the American Medical Association (JAMA).
Study Overview
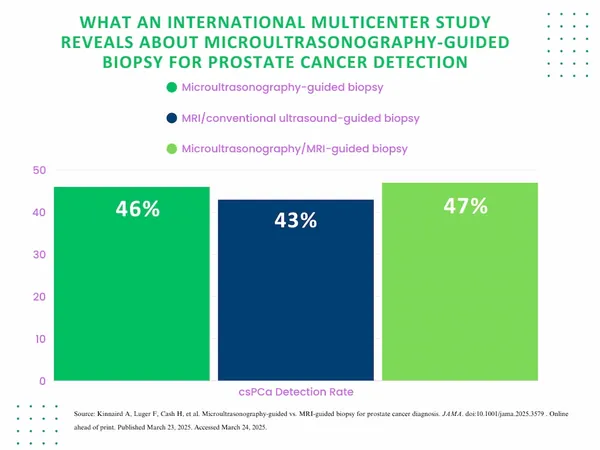
The study, involving 678 men with a median age of 65 and a median prostate-specific antigen (PSA) level of 6.9 ng/mL, assessed the effectiveness of microultrasonography compared to MRI/conventional ultrasound-guided biopsies and a combination approach. Conducted across 20 medical centers, the results revealed that csPCa was detected in 46% of patients using microultrasonography, compared to 43% in those who underwent MRI-guided procedures. A combination of microultrasonography and MRI resulted in a slightly higher detection rate of 47%. However, the differences in detection rates were not statistically significant, indicating that both methods may be equally viable.
Quotes from the Study Lead
Dr. Adam Kinnaird, the lead author from the University of Alberta, emphasizes the implications of these findings: "Microultrasonography could enhance accessibility for patients seeking prostate biopsies, especially those who cannot undergo MRI due to medical contraindications." He highlights that this method simplifies the procedure from a two-step process (pre-biopsy MRI with gadolinium contrast followed by a biopsy) to a single encounter without the need for contrast agents. This change could alleviate patient anxiety, reduce wait times, and lower overall treatment costs.
Advantages of Microultrasonography
Moreover, microultrasonography boasts a remarkable imaging resolution of 70 microns (0.07 mm)—three times better than conventional ultrasound. This advanced resolution facilitates real-time visualization of prostate cancer, minimizing registration errors, and allowing for greater accuracy during biopsy procedures. Such precision becomes crucial, as changes in prostate cancer can significantly alter the ductal architecture.
Considerations and Limitations
While the potential for microultrasonography is promising, researchers caution that a learning curve exists. Physicians involved in the study underwent specialized training in microultrasonography, indicating that this technique requires a higher skill level than traditional methods. Additionally, although various imaging scoring systems exist, the Prostate Risk Identification using Micro-Ultrasound (PRI-MUS) scoring system has only had one iteration so far, suggesting an area ripe for further development.
Study Limitations
However, this study is not without limitations. Researchers noted the absence of blinding concerning the biopsy techniques used, as well as a lack of standardization across different centers for the MRI/ultrasound fusion devices employed. Furthermore, all participants in the study were mandated to undergo biopsy, despite common clinical practices that typically avoid biopsy for men with PI-RADS scores under 3 and favorable PSA levels.
Conclusion
As the medical community continues to explore innovative approaches to prostate cancer detection, microultrasonography stands out as a promising alternative, potentially reshaping how these vital assessments are conducted in healthcare settings across the globe. Will this technology redefine prostate cancer diagnostics? Only time will tell, but the implications of this study are undoubtedly significant for both patients and healthcare professionals alike.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)