Revolutionary Change in Prostate Cancer Diagnosis: Study Finds MRI Can Slash Risks of Unnecessary Cancer Diagnoses
2024-09-25
Groundbreaking Study from GÖTEBORG-2 Screening Trial
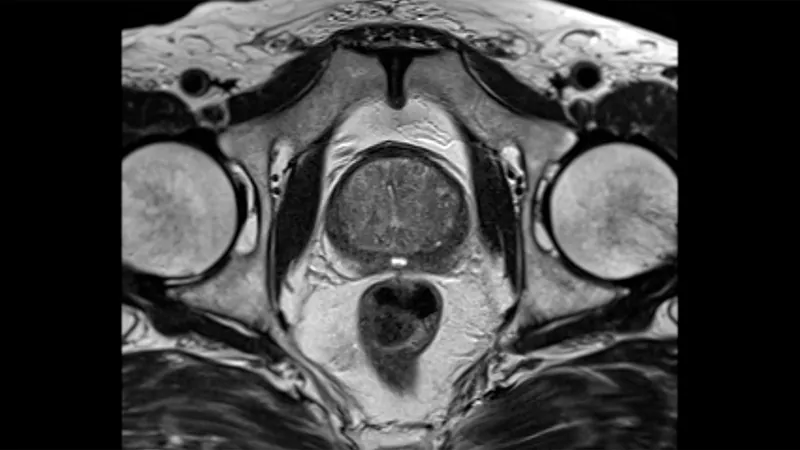
In a groundbreaking study from the GÖTEBORG-2 screening trial, researchers have revealed that omitting systematic biopsy in men with elevated prostate-specific antigen (PSA) levels and negative MRI results can lead to an astonishing reduction of over 50% in the diagnosis of clinically insignificant prostate cancer. This significant finding emerges from four years of follow-up research, which has profound implications for prostate cancer screening and treatment protocols.
Study Findings on MRI-Targeted Biopsies
Dr. Jonas Hugosson and his team from Sahlgrenska University Hospital in Gothenburg reported that the risk of identifying clinically insignificant cancer, either through screening or as interval cancer, was reduced by an impressive 57% in men who underwent MRI-targeted biopsy compared to those who received traditional systematic biopsy. The study’s relative risk was recorded at 0.43, firmly establishing the effectiveness of tailored biopsies for identifying clinically relevant cases while minimizing unnecessary procedures.
Benefits of Repeated MRI Screenings
Notably, the benefits of MRI-targeted biopsies intensify with repeated rounds of screening, yielding an even lower relative risk (0.25) in comparison to the first screening round (0.49). This suggests that MRI not only enhances the accuracy of prostate cancer diagnoses but also significantly decreases the number of men subjected to invasive and potentially harmful biopsy procedures.
Reducing Unnecessary Anxiety and Treatments
Hugosson emphasized, “By omitting prostate biopsies in men who show negative MRI results, we substantially reduce the detection of clinically insignificant cancers, which can lead to unnecessary anxiety, treatments, and active surveillance that may not have been needed.” This finding is especially crucial as it balances the necessity of detecting significant cancers while protecting men from the risks associated with overtreatment.
Rarity of Advanced Cancers in MRI-Targeted Group
The study also drew attention to the rarity of advanced cancers detected among participants: only five cases of very high-risk or advanced metastatic cancer were discovered in the MRI-targeted group versus seven in the systematic biopsy group. This reinforces the idea that most prostate cancers can be effectively visualized by MRI before they escalate into incurable stages.
Interval Cancers and Clinical Significance
Throughout the follow-up period, 42 interval cancers were recorded—17 in the MRI-targeted group and 25 in the systematic biopsy group—with a smaller proportion being clinically significant (six versus fifteen). These results underscore the advantages of adopting MRI technology in clinical settings, where the promise of lower complication rates and more precise diagnostics could transform prostate cancer management.
Expert Recommendations and Future Guidelines
In an editorial accompanying the study, Dr. Paul F. Pinsky of the National Cancer Institute recognized the challenges associated with widespread MRI implementation, but pointed out that this innovative method successfully reduces the number of unnecessary biopsies, saving both resources and lives. “Strategies like these are essential for optimizing prostate cancer screening while preserving its benefits and minimizing harms and costs,” he noted.
Details of the GÖTEBORG-2 Trial
The GÖTEBORG-2 trial involved a robust sample of 13,153 men aged 50 to 60, who were randomly assigned to either the systematic biopsy or the MRI-targeted biopsy pathways. With a median follow-up time of 3.9 years, the researchers focused on clinically insignificant prostate cancer as their primary outcome while also evaluating clinically significant, advanced, and high-risk cancers across both groups.
Conclusion and Future Impact
As this study sets a new standard for prostate cancer diagnosis, the medical community is urged to reevaluate current screening practices. The ripple effect of these findings may shape future guidelines, offering a pathway to a less invasive and more effective approach to managing prostate health. Get ready to rethink prostate cancer screenings—this could change everything!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)