Phage Therapy: A Promising Solution for Superbug Infections Faces Immune System Hurdles
2025-07-02
Author: Daniel
Battling the Rise of Superbugs
As the world grapples with antibiotic-resistant "superbugs," the medical community is increasingly turning to bacteriophages—viruses that specifically target bacteria—as a potential lifesaver. These microscopic predators could revolutionize the treatment of stubborn bacterial infections, but questions linger about their effectiveness when introduced into the human body.
Groundbreaking Study Sheds Light on Phage Therapy
A recent study conducted by teams led by Joshua Weitz at the University of Maryland and Laurent Debarbieux at the Institut Pasteur has uncovered vital insights into the interactions between phages, bacteria, and the immune system. Published in *Nature Communications*, their research focused on the role of phage therapy in treating pneumonia, specifically examining how this innovative approach could enhance clinical outcomes for patients facing multi-drug resistant infections.
Understanding a Complex Relationship
Weitz, a biology professor and data analytics expert, voiced concerns about the escalating health crisis: "The number of antibiotic-resistant infections is skyrocketing, leading to alarming predictions of increased hospitalizations and deaths due to dwindling treatment options." The research utilized animal models to assess how well phages could combat pneumonia caused by *Pseudomonas aeruginosa*, a bacteria responsible for tens of thousands of hospitalizations in the U.S.
The Surprising Role of the Immune System
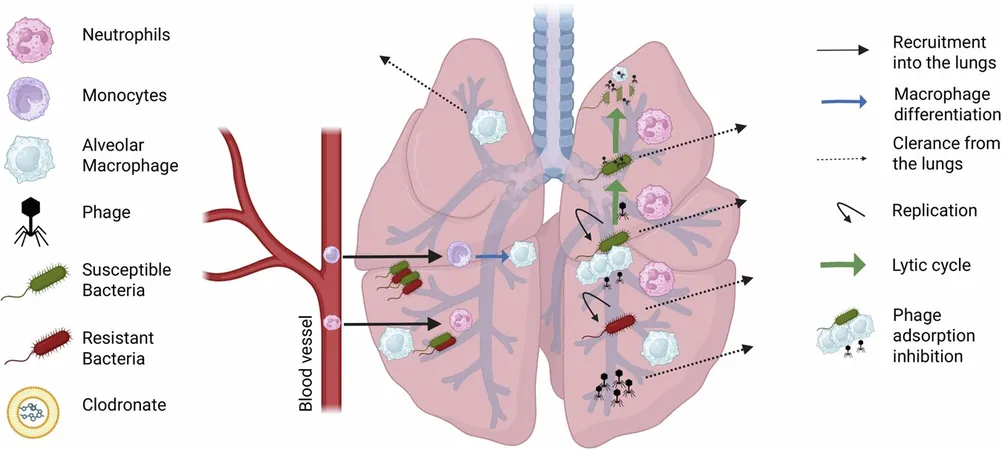
While the concept of phage therapy suggests that introduce phages would directly eliminate harmful bacteria, the reality is far more nuanced. In laboratory settings, phages can quickly diminish bacterial populations, but within the complex environment of a living host, their effectiveness is severely influenced by the immune response.
The study revealed a perplexing finding: immunocompromised animals, particularly those lacking alveolar macrophages—the primary immune defenders in the lungs—actually fared better with phage therapy than their healthy counterparts. Debarbieux noted, "Surprisingly, while these immune cells are crucial for lung protection, their presence may hinder the effectiveness of phage treatment."
Innovative Approaches and Future Research
To delve deeper into this phenomenon, researchers developed a mathematical model that examined the interplay between immune responses, bacterial infections, and therapeutic phages. This model highlighted that alveolar macrophages were inadvertently consuming phages, thus reducing their availability to target bacteria. Debarbieux explained, "In immunocompromised situations, the number of productive phages available for bacterial elimination increases."
These insights stress the complex role the immune system plays during phage therapy. The findings may pave the way for integrating personalized immune system data into treatment plans, ensuring that phage therapy is tailored to each patient's unique circumstances.
Towards a New Era in Therapy Design
Looking ahead, the researchers aim to develop predictive models that can more accurately assess the efficacy of phage therapy under various conditions. This initiative aligns with the goals of the University of Maryland Institute for Health Computing, which seeks to leverage advanced computational techniques to create novel therapeutic strategies against bacterial infections.
As we grapple with the threat of antibiotic resistance, understanding the delicate balance between phages and the immune system could lead to life-saving treatments and a brighter future in the battle against infectious diseases.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)