New Study Reveals Surprising Impact of Beta-Blockers on Heart Failure Patients Exposed to Air Pollution
2025-08-07
Author: Wei Ling
Heart Disease and Air Quality: A Global Dilemma
Particulate matter (PM) is a dangerous air pollutant comprised of tiny particles that pose significant health risks worldwide. In particular, PM2.5, with particles smaller than 2.5 micrometers, is a major public health issue linked to millions of deaths annually. Those suffering from chronic cardiovascular conditions, especially heart failure (HF), find themselves particularly vulnerable to the adverse effects of PM2.5 exposure.
Understanding Heart Failure and Its Risks
Heart failure often stems from various medical conditions including hypertension, ischemic heart disease, and diabetes, leading to chronic strain on the heart. This strain triggers a response in the autonomic nervous system, increasing sympathetic nervous system activation, which can result in serious arrhythmias and further heart damage.
The Role of Beta-Blockers: A Lifeline for Patients?
Beta-blockers, medications prescribed to manage heart failure, work by antagonizing the effects of the sympathetic nervous system. They play a vital role in stabilizing heart rate and reducing blood pressure. However, some studies suggest that the benefits of these medications may interact with environmental factors like PM2.5, raising questions about their effectiveness in high pollution areas.
Exploring the Medication-Environment Interaction
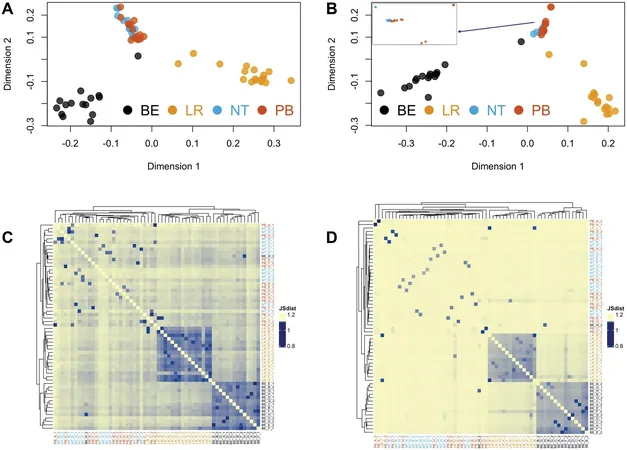
Recent research focused on how beta-blockers influence heart rate and blood pressure in heart failure patients exposed to PM2.5. Utilizing extensive data from North Carolina's heart failure patients, researchers examined the day-to-day cardiovascular impacts of PM2.5 exposure and the role of beta-blocker medications.
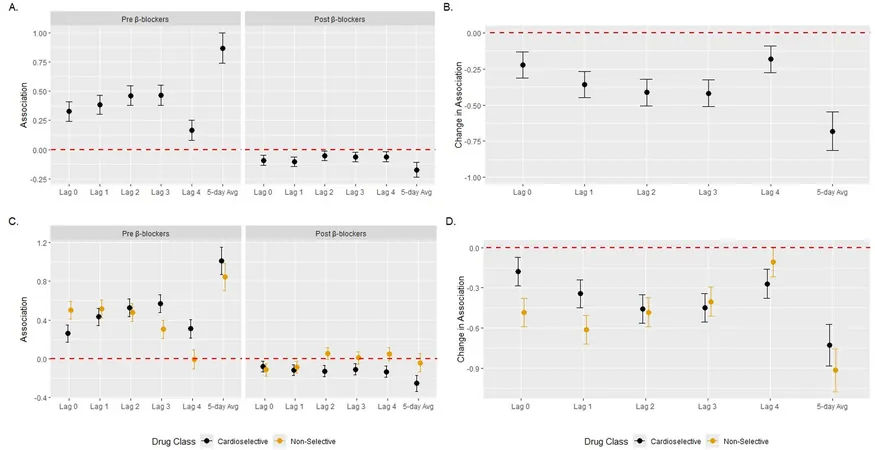
Findings: Mixed Results on Heart Rate and Blood Pressure
The study uncovered that while short-term PM2.5 exposure typically raised heart rates, patients who had been prescribed beta-blockers showed lower heart rates after exposure compared to those who hadn’t. Interestingly, the effects on blood pressure were less predictable, with beta-blockers not consistently mitigating PM2.5-related blood pressure changes.
A Closer Look at Subgroups and Results
Subgroup analyses revealed that women experienced greater reductions in heart rate from beta-blocker use compared to men, pointing to potential biological differences in response to medication. Additionally, white participants showed stronger interactions than their Black counterparts, highlighting possible systemic disparities in healthcare accessibility.
Why This Research Matters
While the findings offer a glimpse into how beta-blockers may protect heart failure patients from the harmful effects of air pollution, more extensive studies are needed. The results underscore the importance of tailored medical care, particularly for vulnerable populations impacted by environmental factors. As air quality continues to be a pressing public health concern, discussions between healthcare providers and patients regarding medication and environmental health risks are more critical than ever.
In Conclusion: A Call for Action and More Research
As urban air quality worsens and heart disease remains a leading cause of mortality, understanding the interactions between medications like beta-blockers and environmental exposures will enhance treatment approaches for heart failure patients. Continued research in this area is essential to identify effective strategies that can mitigate health risks associated with air pollution.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)