New Study Reveals Shocking Truth About Pain Management in Older Adults After Hip Fractures – What You Need to Know!
2024-10-30
Author: Nur
In an era where pain management is paramount, a groundbreaking analysis has emerged from a proof-of-concept study focusing on older adults receiving care in skilled nursing facilities (SNFs) after suffering hip fractures. This research underscores the critical importance of effective analgesic regimens during the post-acute care period, which can make or break a patient's functional recovery and prevent severe complications like delirium and increased disability.
Understanding the Need for Pain Management
When older adults experience hip fractures—a common yet debilitating injury—the transition from hospital to rehabilitation in SNFs is often accompanied by severe pain. Pain management during this transition is not just about comfort; it has far-reaching implications on recovery times and overall quality of life. Untreated or poorly addressed pain can lead to missed physical therapy sessions, complicating recovery.
Currently, guidelines advocate for multimodal analgesia—using different medications to manage pain more effectively—but they lack specificity regarding the safest and most effective combinations for older populations. Given the vulnerabilities associated with aging and polypharmacy, it’s crucial to identify which analgesics are being used in these facilities.
Medicare’s Influence on Medication Reporting
Most SNF patients are covered by Medicare, yet the existing prescription drug claims data often fails to capture the real story of pain management during SNF stays. The restrictions of Medicare Part D during institutional care lead many studies to miss vital insights into medication usage during the rehabilitation period. As a result, most existing research has focused on analgesic administration during the initial hospitalization rather than the critical post-acute stage.
Innovative Data Collection Methods
This study sought to overcome these challenges. Researchers from Brown University successfully harmonized Electronic Health Record (EHR) data from multiple SNF chains, creating a federated database that includes nearly 700 facilities across the U.S. They meticulously analyzed medication use and patterns among residents with hip fractures, which many previous studies had overlooked.
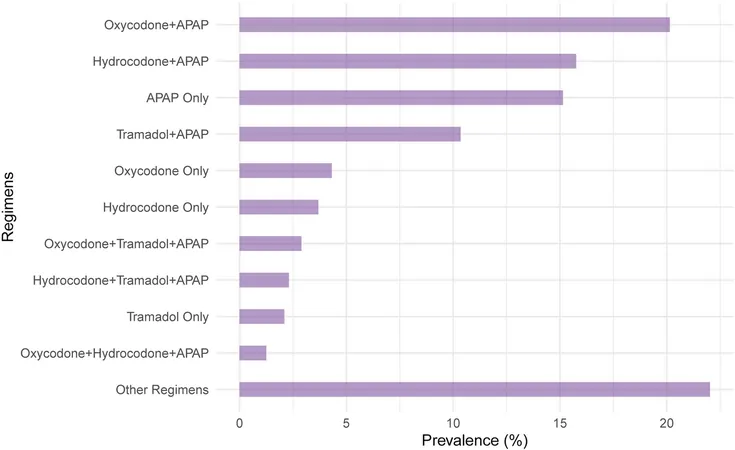
Key Findings: Almost 60% Use Opioids + APAP
Between January 2018 and June 2021, the analysis revealed that approximately 60% of residents used a combination of opioids and acetaminophen (APAP), marking a substantial reliance on this regimen for post-fracture pain management. Other common combinations included hydrocodone with APAP and tramadol with APAP. Interestingly, the use of non-prescription analgesics like ibuprofen was rarely documented, raising questions about the comprehensive nature of pain management strategies in these settings.
Moreover, a notable increase in the use of APAP-only regimens among patients with cognitive impairments suggests an evolving approach to pain relief, particularly post the onset of the COVID-19 pandemic. However, reliance on opioids remains consistently high due to their effectiveness in managing acute pain.
Trending Changes in Analgesic Use Post-Pandemic
The COVID-19 pandemic profoundly altered healthcare practices, including pain management in SNFs. This study's results hinted at shifting trends in medication prescribing, with some combinations experiencing increased prevalence while others, like certain hydrocodone regimens, showed a decline following the onset of the pandemic.
Conclusion: A Call for Future Research
This innovative study not only sheds light on the current state of analgesic prescribing but also emphasizes the need for further research. Identifying the safest and most effective pain management strategies will be crucial, especially in a vulnerable demographic that may experience adverse effects from commonly prescribed medications.
In conclusion, as we advance in our understanding of pain management for older adults, the findings from this proof-of-concept study highlight an urgent need for ongoing education and adaptation in our practices to enhance recovery and quality of life for those recovering from hip fractures. The data gathered serves as a vital resource for future studies aimed at optimizing analgesic use and addresses significant gaps left by traditional data reporting mechanisms. If you or a loved one is navigating recovery from a hip fracture, understanding these findings could be critical to ensure effective pain management strategies are implemented.
 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)