Alarm Over Rising Partial Resistance to Artemisinin in Malaria-Causing Parasites in Uganda: New Study Raises Concerns!
2024-11-05
Author: Daniel
Background
In the battle against malaria, artemisinin-based combination therapy (ACT) has been hailed as the frontline treatment, crucial for managing uncomplicated malaria. However, a troubling new study reveals a disturbing trend: the emergence of partial resistance to artemisinin in the Plasmodium falciparum parasite, particularly in high-transmission areas of Uganda. As experts scramble to address this issue, the implications for malaria control in sub-Saharan Africa—where the disease burden is most severe—are alarming.
Methods
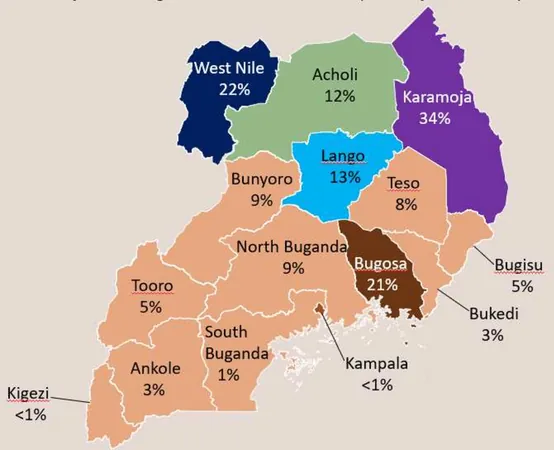
To understand the extent of this emerging resistance, health researchers conducted a comprehensive genomic surveillance study at 50 sites across Uganda's Karamoja, Lango, Acholi, and West Nile regions from June 2021 to August 2023. The study involved diagnosing symptomatic malaria patients and collecting dried blood spots for advanced genomic analysis. A total of 563 dried blood samples were scrutinized, with 240 being further selected to search for pfk13 mutations, known markers of partial artemisinin resistance.
Results
Out of the tested samples, an astonishing 99.2% contained sufficient DNA to yield conclusive results, revealing several concerning mutations. The study identified three noteworthy pfk13 mutations: C469Y (present in 13.5% of samples), A675V (5.9%), and S522C (only in one sample). Alarmingly, the frequency of the C469Y mutation reached 23.3% in the Karamoja region, which significantly outpaced other areas. Conversely, the West Nile region exhibited a predominance of wild-type strains, indicating a stark regional disparity.
Conclusion
These findings underscore the critical need for ongoing genomic surveillance to assess and monitor the rise of artemisinin resistance in Uganda. The findings serve as a stark warning that, without proactive efforts to identify and manage these mutations, the progress made in malaria control could swiftly unravel. Health officials are urged to reconsider current treatment policies and reinforce containment strategies, as any delay in response could lead to widespread treatment failures.
The Bigger Picture
Malaria continues to plague Uganda, accounting for 5.4% of the global malaria cases reported in 2022, making it the third largest contributor to this public health crisis worldwide. With a population vulnerable to infection, malaria transmission varies widely across regions, complicated by factors such as public health efforts, socioeconomic status, and drug accessibility. While Uganda's national malaria strategies have improved access to long-lasting insecticide-treated nets and subsidized ACTs, the recent stagnation in progress raises concerns.
Additionally, cases of partial artemisinin resistance have been documented for the first time on the African continent, with escalating reports from neighboring countries including Rwanda and Tanzania. This is especially worrying as similar resistance patterns experienced in Southeast Asia could potentially threaten decades of progress made against malaria in Africa.
In response, the World Health Organization (WHO) has initiated comprehensive strategies to manage artemisinin resistance across the continent, emphasizing the need for robust surveillance and regional cooperation to combat this dire threat. However, the presence of mutations in the pfk13 gene complicates these efforts, potentially yielding increased transmission, prolonged infection, and heightened risks of mortality.
A Call to Action
The emergence of validated markers of artemisinin partial resistance in Uganda's malaria landscape demands urgent intervention. Stakeholders must prioritize enhanced molecular surveillance, rigorous monitoring of treatment efficacy, and strict regulations on the distribution of anti-malarial medications. With the looming threat of a resurgence in malaria transmission and deterioration of treatment outcomes, a unified and proactive response is essential to safeguard public health in Uganda and beyond.
This study illustrates a pivotal turning point in malaria control—one that has the potential to redefine treatment protocols and reshape public health strategies in response to evolving threats. Will Uganda's response be proactive enough to avert a public health catastrophe? Only time will tell.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)