New Research Reveals Groundbreaking Insights into Overcoming Drug Resistance in Pancreatic Cancer
2024-11-07
Author: Ming
New Research Reveals Groundbreaking Insights into Overcoming Drug Resistance in Pancreatic Cancer
In a significant breakthrough, researchers from the University of Virginia (UVA) have unveiled a new mechanism that contributes to drug resistance in pancreatic ductal adenocarcinoma (PDAC), one of the most lethal forms of cancer. Their groundbreaking findings have been published in the prestigious journal *Cancer Research* and could pave the way for more effective treatment strategies, offering much-needed hope to patients battling this aggressive disease.
Understanding the Deadly Link Between Hypoxia and Cancer Aggression
Pancreatic tumors are infamously resistant to chemotherapy largely due to their dense structure and poor blood supply, creating areas of low oxygen, or hypoxia. Professor Matthew J. Lazzara, who is based in both the Department of Chemical Engineering and the Department of Biomedical Engineering at UVA, led a team to explore whether this hypoxic environment causes cancer cells to become more aggressive and resistant to treatment.
“Our inquiry was straightforward: Do low-oxygen conditions in pancreatic tumors lead to increased chemotherapy resistance in cancer cells, and do they activate the same pathways as those stimulated by growth factors?” Lazzara explained.
Growth factors, which are naturally occurring proteins in the body, often aid in cellular growth and survival. However, in the context of cancer, they can also enhance tumor progression and facilitate evasion from treatments like chemotherapy.
Revealing a Long-Lasting Mechanism of Resistance
The team's shocking discoveries indicated that hypoxia not only promotes a more aggressive cancer cell state but that this change is significantly more sustainable than the modifications spurred by growth factors. This durability presents a substantial obstacle for effective treatment options.
The research demonstrated that when exposed to low oxygen levels, pancreatic cancer cells undergo a specific process that alters their genetic material and cellular signaling pathways, rendering them more resilient against chemotherapy. Critically, these hypoxia-induced transformations can persist for weeks, complicating treatment efforts long after the initial low-oxygen exposure.
“We have identified multiple potential strategies to disrupt and even reverse this resistant state in cancer cells,” said Brooke Brown, a collaborator on this pivotal study.
Innovative Tracking Techniques for Enhanced Understanding
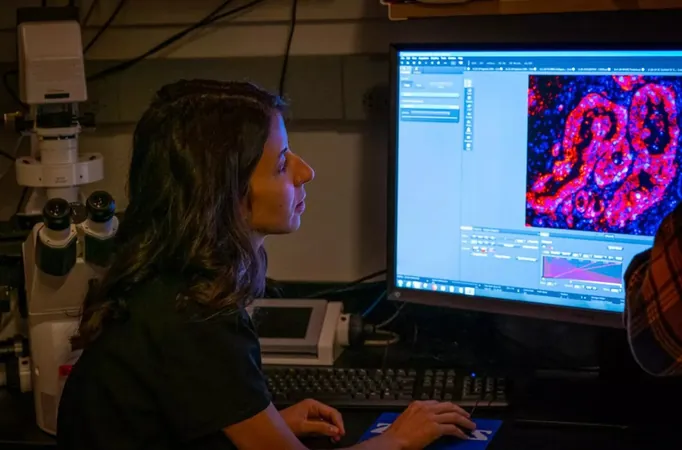
To investigate how hypoxia affects pancreatic cancer cells, the researchers utilized an innovative hypoxia lineage tracing system developed by experts at Johns Hopkins University. This cutting-edge approach enabled them to monitor the effects of low oxygen exposure on cancer cells over time, corroborated by various data sources, including in vitro models, numerous animal models, and comprehensive computational analysis of human patient data.
“This methodology was revolutionary as it combined cell culture, animal studies, and computational modeling to deeply understand how hypoxia contributes to chemoresistance,” Lazzara highlighted.
What This Means for the Future of Treatment
The next phase of research will focus on how these previously identified pathways react when subjected to chemotherapy drugs, which can inadvertently promote resistance. Additionally, Lazzara’s team is investigating the roles other cells in the tumor microenvironment, such as fibroblasts, play in relation to hypoxia.
This impactful study offers a significant advancement for the treatment of pancreatic ductal adenocarcinoma. With strategies aimed specifically at counteracting the persistent, hypoxia-induced modifications in cancer cells, there is a promising possibility for developing more effective therapies. Such targeted approaches could drastically improve treatment outcomes and survival rates for individuals facing this formidable disease, potentially transforming the landscape of pancreatic cancer treatment.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)