New Evidence Reveals NO Superior Advantage of Intraosseous Access in Cardiac Arrest Treatment
2024-10-31
Author: Ming
Introduction
In a significant development for emergency medical practices, two large-scale randomized trials have shown that intraosseous vascular access—commonly used for the administration of epinephrine during out-of-hospital cardiac arrests—does not confer a survival advantage over traditional intravenous (IV) access as the first line of treatment.
Study Overview
Conducted in the U.K. and Denmark, respectively, the PARAMEDIC-3 and IVIO trials brought together data from over 7,500 patients experiencing cardiac arrest. Findings from the PARAMEDIC-3 trial, led by esteemed researcher Gavin D. Perkins from University Hospitals Birmingham NHS Foundation Trust, revealed a meager 30-day survival rate of 4.5% when intraosseous access was the initial choice, compared to 5.1% for those receiving IV access first (Adjusted Odds Ratio: 0.94, P=0.74).
Similarly, the Danish IVIO trial, led by Lars W. Andersen from Aarhus University Hospital, echoed these sentiments by demonstrating nearly identical outcomes in terms of sustained return of spontaneous circulation and overall survival. In the IVIO study, the rates stood at 30% for intraosseous access versus 29% for IV access (Risk Ratio: 1.06), also failing to show significant differences.
Presentation of Findings
Both studies were presented at the European Resuscitation Council Congress in Athens and subsequently published in the prestigious New England Journal of Medicine. Their complementary findings have led experts, including Niklas Nielsen from Lund University, to state that current guidelines recommending an IV-first strategy remain justified, but the evidence supporting it has gained strength.
Discussion
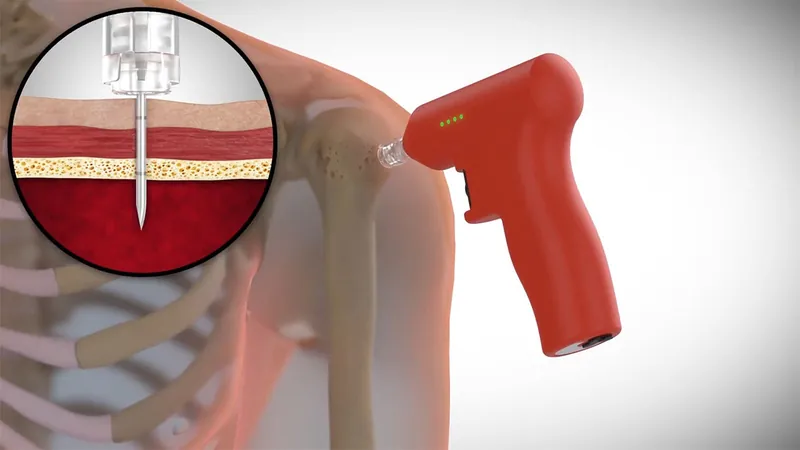
Despite the rapidity of intraosseous access—which can be achieved by inserting a cannula into the spongy tissue of a bone—the results suggest that outcomes could be more favorable with IV administration, particularly in achieving a sustained return of spontaneous circulation. In the PARAMEDIC-3 trial, a notable secondary endpoint revealed that 39.1% of those receiving IV access experienced a return of circulation at any stage, compared to only 36.0% in the intraosseous group.
Interestingly, the IVIO trial also reported significantly higher rates of successful vascular access within two attempts—92% for the intraosseous group and 80% for the intravenous group—indicating that while intraosseous access may be technically easier, it does not translate into better survival rates.
Limitations and Conclusion
Both trials faced limitations, particularly the inability to blind emergency medical crews to the access route employed, raising potential concerns regarding bias. Nevertheless, the rigor of CPR standardized protocols minimized these biases, leading to a consensus on the findings.
As resuscitation practices continue to evolve, these trials usher in a refreshed discourse around the optimal approach for emergency medical personnel. The medical community now stands at a crossroads: with compelling evidence emerging, will there be a shift back to prioritizing intravenous access in life-or-death scenarios? The debate is just beginning—stay tuned for more updates as this pivotal story unfolds.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)