
Groundbreaking Discovery in Breast Cancer Treatment: NUS Researchers Revolutionize Chemotherapy with Magnetic Fields
2025-01-07
Author: Sarah
Recent findings from the National University of Singapore (NUS) have sparked excitement in the medical community as researchers unveil an innovative, non-invasive approach to enhance chemotherapy effectiveness and mitigate its notorious side effects.
Singapore, January 7, 2025
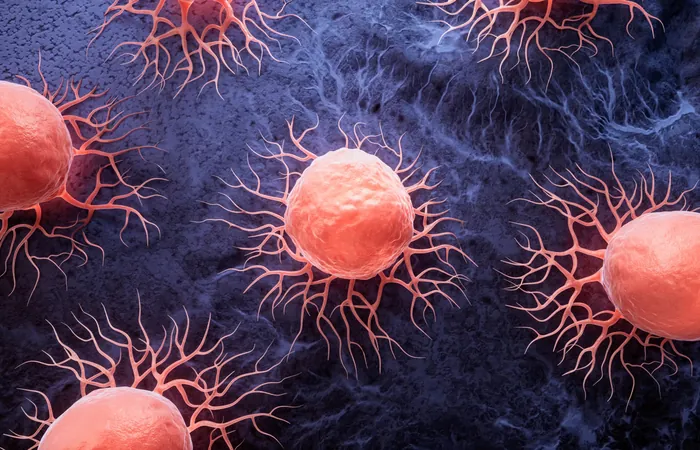
A study conducted by a team at NUS has revealed that employing targeted magnetic fields can significantly improve the uptake of doxorubicin (DOX), a crucial chemotherapy drug widely used in breast cancer treatment. This method not only targets cancer cells more effectively but also preserves healthy tissues, potentially reshaping the landscape of cancer therapies.
Unlocking the Mechanism: Magnetic Fields in Action
The research, led by Associate Professor Alfredo Franco-Obregón at NUS's Institute for Health Innovation & Technology (iHealthtech), is pioneering in demonstrating how pulsed magnetic fields enhance the absorption of DOX in breast cancer cells. The findings, published in the journal Cancers on November 18, 2024, are built on previous 2022 research that indicated certain cancer cells' heightened susceptibility to magnetic field therapies.
DOX operates by disrupting DNA replication and cellular respiration, leading to cancer cell death. However, one significant drawback is its non-selective nature, which can cause severe side effects ranging from heart issues to muscle wasting. This new method presents an exciting solution by enhancing drug uptake in targeted cells while protecting healthy tissues.
How It Works: The Role of TRPC1 Channels
The researchers pinpointed the calcium ion channel TRPC1 as a critical factor in this process. Found commonly in aggressive cancer types, TRPC1 is activated by magnetic field exposure, facilitating the transport of DOX into cancer cells. In experiments, breast cancer cells exposed to magnetic fields absorbed significantly higher DOX levels compared to normal muscle cells, resulting in more efficient cell death in tumors.
Moreover, within just 10 minutes of magnetic exposure, the drug concentration needed to kill cancer cells was reduced by half, emphasizing the potential for lower doses of chemotherapy that could diminish systemic toxicity. The cancerous cells responded well, while healthy cells remained largely unharmed.
A Breath of Fresh Air for Cancer Patients
With breast cancer being the leading cause of cancer death among women globally, the urgency for innovative treatments has never been more pronounced. Many women experience severe side effects from traditional chemotherapy, which sometimes necessitates dose adjustments or discontinuation altogether. Assistant Professor Joline Lim, a member of the research team, highlighted the critical need for such targeted approaches, which could significantly enhance patient outcomes and well-being.
In a world where drug resistance due to prolonged high-dose chemotherapy treatments is a reality, this research marks a monumental advancement in precision oncology.
Future Directions: From Lab to Clinic
Looking ahead, the research team is committed to fine-tuning this magnetic-assisted therapy for clinical application. Their goal is to localize magnetic field exposure directly to tumors in patients, maximizing drug delivery precisely where it is needed while minimizing side effects.
The dynamic team is also in the process of patenting their groundbreaking technique and exploring opportunities to launch a startup focused on breast cancer treatment, signaling a promising pathway to transform treatment paradigms. Investors in Southeast Asia and the United States are already showing interest, highlighting the potential global impact of their discoveries.
In Summary
With a method that could change the face of breast cancer treatment, NUS researchers have paved the way toward a future where chemotherapy can be both effective and less burdensome. As we await clinical trials, the hope for patients is becoming increasingly tangible, potentially ushering in a new era of cancer care that prioritizes precision and quality of life.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)