Faricimab's Promise for Macular Degeneration Unfulfilled, Raises Questions on Efficacy
2024-12-30
Author: Rajesh
Introduction
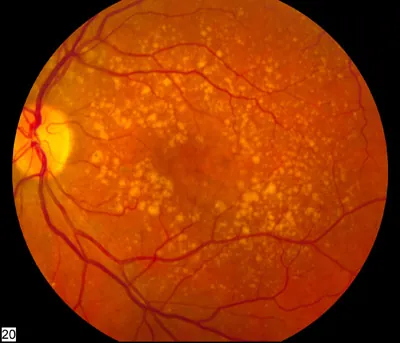
In a significant development for the treatment of macular degeneration and related visual impairments, faricimab has recently been approved for use in Europe. This approval, which came into effect in July 2024, allows the drug to be prescribed for visual impairment stemming from macular edema secondary to retinal vein occlusion. However, an investigation by the German Institute for Quality and Efficiency in Health Care (IQWiG) has raised serious concerns regarding the actual benefits of faricimab in comparison to existing therapies, namely ranibizumab and aflibercept.
Concerns Raised by IQWiG
Despite the promising introduction of faricimab, the drug manufacturer has failed to provide sufficient data demonstrating its effectiveness over these established treatments. As a result, IQWiG has concluded that there is no substantiated added benefit of faricimab when compared to its counterparts.
Trial Data and Protocol Issues
The manufacturer submitted data from two randomized controlled trials (RCTs), known as BALATON and COMINO, which involved comparisons between faricimab and aflibercept. However, key issues emerged: the treatment protocols used in these studies deviated from the specifications outlined in the Summary of Product Characteristics. Patients were treated continuously even when their conditions showed signs of stability, and the flexibility to customize dosing regimens was absent during the primary phase of comparison between the two drugs.
Treatment Regimen Concerns
Typically, the appropriate treatment regimen for both faricimab and aflibercept involves initial administration every four weeks, with the potential for three or more consecutive monthly injections, followed by a personalized ‘treat-and-extend’ approach reliant on the observed disease activity.
Stabilization and Treatment Adjustments
Alarmingly, data revealed that a significant number of patients in the BALATON and COMINO studies had reached stabilized condition within just 8 to 12 weeks. Unfortunately, individual adjustments to the treatment were only permitted starting from Week 24, well after the initial stabilizations had occurred. This raises critical questions about the effectiveness of the treatment regimens being followed, as many patients remained on unchanged treatment protocols despite showing stable findings.
EMA Recommendations Ignored
Further complicating matters, the European Medicines Agency (EMA) recommended that the manufacturer conduct a study employing a treat-and-extend dosing regimen across both study arms. This guidance was notably disregarded, suggesting a potential oversight in the pursuit of data integrity.
Comparative Efforts in Other Trials
In contrast, the RCT TALON, which evaluates the efficacy of brolucizumab against aflibercept in treating wet age-related macular degeneration, successfully incorporated a treat-and-extend regimen for both treatment arms. This design allowed for individual treatment intervals to be adjusted according to each patient’s disease activity, thereby strengthening its suitability for benefit assessment, which was finalized in early 2024.
Conclusion and Future Implications
As the landscape of macular degeneration treatments continues to evolve, the implications of faricimab’s benefit assessment and the choices made by its manufacturer may prompt patient advocates and healthcare professionals to reconsider treatment options. Are patients being protected by following through with therapies that lack substantial evidence of enhanced efficacy? Only time will tell if the decisions made today will reshape the future of macular degeneration treatment.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)