Exploring the Link Between Cognitive Decline, White Matter Changes, and Suicide Risk in Elderly Depression Patients
2025-09-03
Author: Wei Ling
Unlocking the Mystery of Late-Life Depression and Suicide Risk
In a groundbreaking exploratory study, researchers scrutinized the intricate web of cognitive decline, white matter hyperintensities (WMH), and suicide risk among elderly patients grappling with major depression. The study surveyed 58 participants aged 65 and above, focusing on three distinct groups to unveil critical insights.
Diving into the Participant Groups
The first group, labeled as Recent Suicide Attempt (RSA) patients, included individuals from a psychiatric inpatient setting who had recently engaged in self-harming behaviors with suicidal intent. These individuals were rigorously assessed and diagnosed according to DSM-5 standards by psychiatric specialists.
The second group, Non-Suicidal (NS), consisted of patients diagnosed with major depression but devoid of self-harm or suicidal thoughts. Finally, a healthy control (HC) group was recruited to provide a baseline for cognitive functioning, comprising older adults with no significant psychiatric or neurological histories.
A Comprehensive Evaluation Framework
The study implemented a variety of cognitive and clinical assessments, including the Cognitive Abilities Screening Instrument (CASI), which gauges cognitive function across nine domains. Participants had to meet specific cognitive thresholds to ensure the integrity of the study.
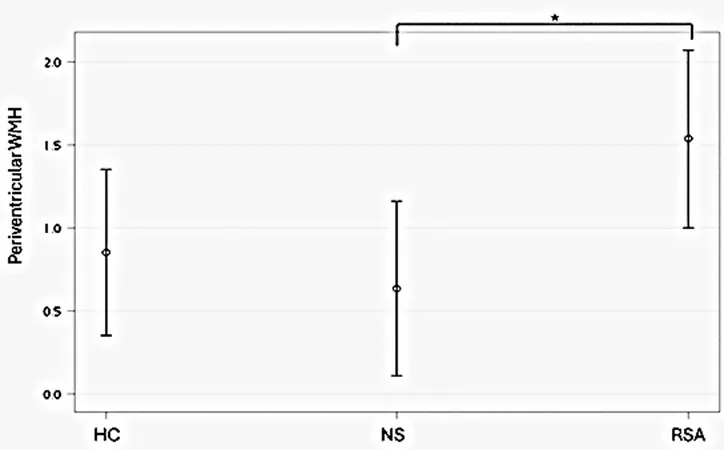
MRI Insights Reveal White Matter Hyperintensities
MRI scans were pivotal in the research, where T2-weighted FLAIR sequences assessed the severity of WMH. The findings indicated that RSA patients exhibited significantly elevated WMH burden, particularly in the periventricular regions, compared to both the NS and HC groups.
Cognitive Function: A Concerning Trend
Strikingly, RSA patients displayed markedly lower cognitive function, particularly concerning attention and orientation, compared to their healthy counterparts. This decline in cognitive abilities not only highlights the challenges faced by these individuals but also raises alarms about their increased suicide risk.
Linking WMH to Suicide Risk
The connection between higher WMH loads and decreased cognitive function among RSA patients sheds light on potential biomarkers for suicide risk in late-life depression. This relationship emphasizes the urgent need for further investigation into how WMH may influence emotional regulation and cognitive processing, making older adults more vulnerable to suicidal crises.
A Call for Future Research
While this study offers valuable insights, it also calls for caution due to its exploratory nature and limited sample size. Future research is essential to explore these findings further and consider the complexities of cognitive function, WMH, and suicide risk among various demographic segments, particularly elderly men who are often underrepresented due to stigma.
In conclusion, as this study reveals compelling connections between cognitive decay, WMH, and suicide risk in late-life depression, it paves the way for a deeper understanding of mental health dynamics and potential interventions for at-risk elderly populations.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)