Diabetes and Albuminuria: A Double-Edged Sword in Heart Failure with Preserved Ejection Fraction
2025-04-05
Author: Li
Introduction
Heart failure with preserved ejection fraction (HFpEF) is a common condition with a significant metabolic component. A growing body of evidence highlights the critical roles of diabetes mellitus and albuminuria—an early marker for kidney disease—in contributing to adverse health outcomes for patients battling this condition. Understanding how these factors interplay can be vital for improving patient management and minimizing risk.
Study Overview
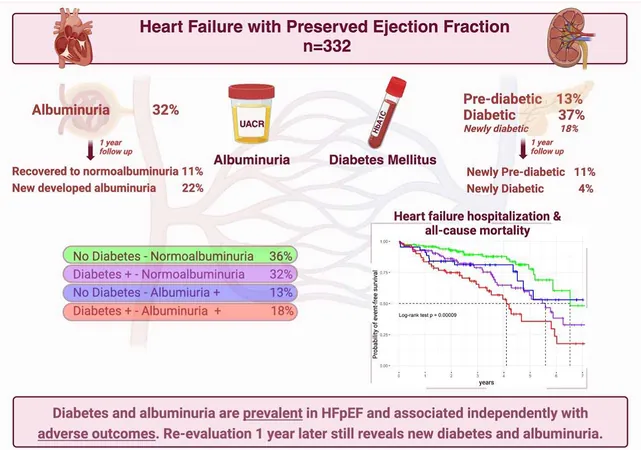
This study followed 332 patients diagnosed with HFpEF from March 2015 to November 2023. It specifically examined the prevalence and prognostic impact of both diabetes and albuminuria—two prevalent comorbidities within this patient population. Notably, patients with type 1 diabetes were excluded from the analysis to ensure a clearer focus.
Participants were categorized based on their glucose metabolism status and albuminuria levels. The primary outcome assessed was a composite of heart failure hospitalizations and overall mortality, evaluated through advanced statistical models.
Key Findings
The patient cohort had a median age of 77, with 67% being women. Disturbingly, 63% of patients presented with some form of impaired glucose metabolism (either diabetes or prediabetes), and 31% exhibited albuminuria.
The analysis revealed that both diabetes and albuminuria independently predicted adverse outcomes within approximately three years. The most alarming statistic was that patients falling into the DM+/ALB+ category had a staggering 186% higher risk for negative outcomes compared to those who lacked both conditions.
Temporal Changes and Implications
Interestingly, upon re-evaluation after one year, new cases of diabetes were observed in 3.9% of previously non-diabetic patients, while a shocking 22% developed new incidences of albuminuria. This indicates that routine screening could potentially change management strategies for at-risk patients, given how frequently new cases emerged.
At a three-year follow-up, the individuals who consistently had albuminuria or who had developed it during the year experienced the highest rates of adverse outcomes at 27.1% and 13.9%, respectively. The data underscore the pressing need for consistent monitoring of glucose metabolism and albumin levels in patients with HFpEF.
Clinical Implications
Given the significant correlation between diabetes, albuminuria, and heart failure outcomes, this study lends weight to the argument for routine screening for blood sugar and kidney function in individuals diagnosed with HFpEF. This approach could lead to earlier therapeutic interventions and potentially improve clinical outcomes.
Conclusion
As HFpEF continues to plague healthcare systems around the globe, integrating assessments for diabetes and albuminuria into routine care may be pivotal for identifying patients at heightened risk and improving overall management strategies. With studies like this highlighting the time-sensitive nature of these conditions, clinicians must take proactive steps to mitigate risks, thereby enhancing patient care.
The findings ultimately indicate the need for increased awareness and screening for diabetes and kidney dysfunction among HFpEF patients, bringing new urgency to the management of these intertwined conditions.
Are you or someone you know battling HFpEF? Stay informed and monitor these crucial health markers to safeguard your health!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)