Breakthrough: Stanford's CAR-T Cell Therapy Revolutionizes Treatment for Lethal Childhood Brain Cancer
2024-11-13
Author: Wei Ling
Introduction
In a groundbreaking clinical trial at Stanford Medicine, researchers have found that an innovative immune-cell therapy significantly shrank brain tumors in children, restored neurological functions, and, in an extraordinary case, erased all detectable traces of a normally incurable brain cancer known as diffuse intrinsic pontine glioma (DIPG). The promising results are a part of ongoing research aimed at transforming the grim landscape of pediatric brain cancers.
Publication and FDA Designation
Published online on November 13 in the prestigious journal *Nature*, this study is among the first to document successes in treating solid tumors with engineered immune cells called CAR-T (Chimeric Antigen Receptor T) cells. The U.S. Food and Drug Administration (FDA) has already recognized this therapy with a Regenerative Medicine Advanced Therapy designation, paving a potentially expedited path to approval due to its remarkable promise.
Trial Results
In the trial involving 11 young participants, 9 reported positive results. Notably, four of them experienced tumor size reductions exceeding 50%, and one patient, Drew, witnessed a complete disappearance of his tumor—a milestone in the struggle against this deadly disease. Although it remains uncertain if he is entirely cured, Drew is currently thriving, four years post-diagnosis.
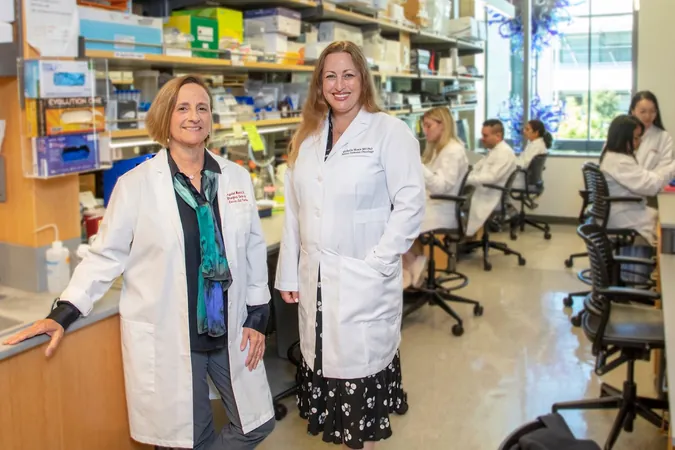
Expert Insights
“This is a universally lethal disease, and we have uncovered a treatment that leads to meaningful tumor regressions and clinical improvements,” stated Michelle Monje, MD, PhD, the leading author and Professor of Pediatric Neuro-Oncology at Stanford. “Although optimizing this treatment for all patients is our next challenge, it's exhilarating that we have achieved a complete response in one case.”
Drew's Diagnosis
Drew's journey began in November 2020 during his junior year of high school when a series of alarming symptoms—a combination of headaches, partial paralysis, and unusual eye movements—led to his devastating diagnosis. DIPG affects the brainstem, intermingling malignant cells with healthy nerve structures, making surgery impossible. With a median survival time of only a year, radiation offers fleeting respite, and no effective chemotherapy exists.
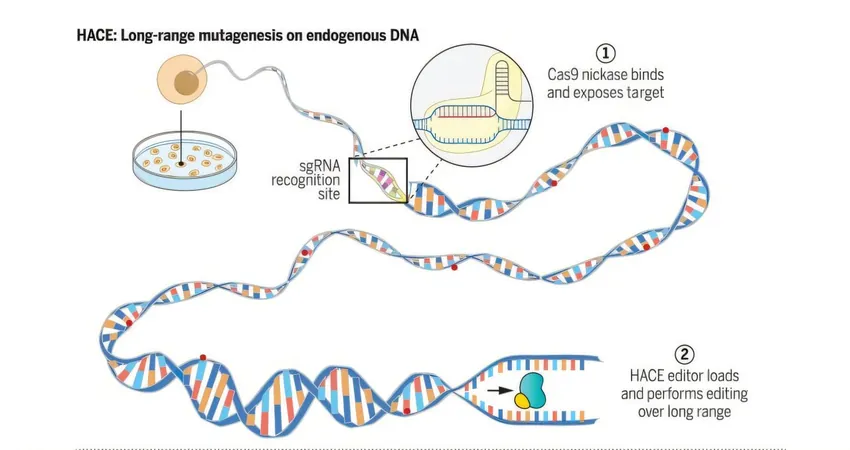
Research Aims
The study demonstrates a radical shift in outlook for this subset of pediatric patients. Researchers had previously approached the trial with cautious optimism, having found encouraging results in animal models. The developed CAR-T cells specifically target a surface marker known as GD2, abundant in DIPG and similar tumors.
Tailored Treatment Approach
The trial focused on crafting a tailored approach for each patient, establishing a safe dose of the therapy, and closely monitoring side effects. Initial infusions reflected the side effects common to cytokine release syndrome, but subsequent infusions safely delivered the CAR-T cells into the cerebrospinal fluid, contributing to positive neurological outcomes and improved tumor responses.
Drew's Recovery
Drew's inspirational recovery story is a testament to the potential of this therapy. After undergoing several CAR-T cell infusions and overcoming initial side effects, he defied expectations—graduating high school in May 2022 without assistance and continuing to improve. Drew is now thriving in college, majoring in forestry, while still receiving CAR-T treatments and enjoying life unburdened by his past illness.
Drew's Perspective
"I'm determined to pursue my interests in conservation and rewilding," Drew shared. "It's amazing to think that my experience might help pave the way for other children battling cancer."
Ongoing Research
Researchers continue to scrutinize biological samples from trial participants to further refine the therapy and identify factors that influenced different outcomes. The long-term vision remains clear: to minimize treatment toxicity while enhancing benefits for all patients facing similar diagnoses.
Family Gratitude
Drew's family expresses immense gratitude for the groundbreaking research that led to this therapy, underscoring the importance of shared human experiences in furthering medical advancements.
Conclusion
This pioneering study is not just a beacon of hope for families grappling with childhood brain cancer, but it signals a broader promise for the future of immunotherapy in treating central nervous system cancers. Stay tuned to see how this revolutionary therapy might change the face of pediatric oncology!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)