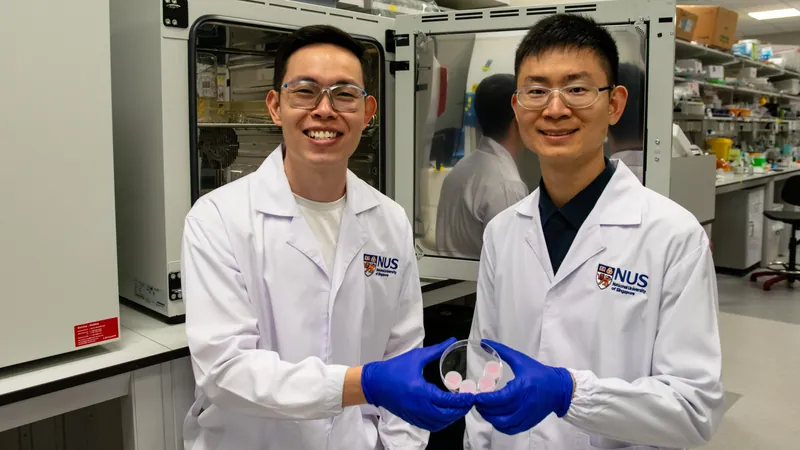
Breakthrough Microneedle Technology from NUS Set to Revolutionize Diabetic Wound Healing
2025-03-26
Author: Daniel
Diabetic Wounds and Their Impact
Diabetic wounds pose a serious threat to health and wellbeing, often leading to complications such as infections and, regrettably, amputations. Alarmingly, these chronic, non-healing wounds affect over six percent of the global population, with Singapore alone witnessing about four lower limb amputations each day linked to this dire condition. A study conducted in Singapore highlighted the staggering financial burden of such healthcare interventions, estimating the cost per patient for amputation-related care at an eye-watering S$23,000 in 2017.
Innovative Microneedle Technologies
In a significant leap toward alleviating this crisis, researchers at the National University of Singapore (NUS) have unveiled two innovative microneedle technologies that have demonstrated impressive efficacy in accelerating wound healing in preclinical models. These technologies work by preserving vital growth factors and eliminating harmful inflammatory compounds from the wound area.
The research team was spearheaded by Assistant Professor Andy Tay from the Department of Biomedical Engineering at NUS, collaborating with the Institute for Health Innovation and Technology. "Growth factors are essential for wound healing as they regulate various cellular functions," explained Professor Tay. "However, in diabetic wounds, these factors are quickly degraded by proteases, which drastically impedes recovery. Additionally, persistent inflammation characterizes these wounds."
Two Innovative Approaches to Enhance Wound Healing
Currently, hydrogel therapies are employed to deliver growth factors to wounds, but these methods often fall short due to the protease-rich environment that leads to premature degradation. Instead, NUS researchers took a bold approach by first enhancing the body's natural production of growth factors at the wound site.
Their first innovation involves sucralfate microneedles (SUC-MN) that deliver interleukin-4 (IL-4), a potent immunomodulatory protein. IL-4 encourages the production of essential growth factors within diabetic tissues while sucralfate—a commonly used medication for gastrointestinal ulcers—safeguards these factors from degradation. These microneedles dissolve upon contact with the wound, ensuring localized delivery and minimizing systemic side effects. Remarkably, the researchers found that SUC-MN accelerated wound healing at twice the rate compared to traditional treatment methods.
In an unprecedented move, the NUS team also explored the potential of microneedles to extract unwanted pro-inflammatory compounds. For this purpose, they developed heparin-coated porous microneedles (HPMN), designed to trap and remove chemokines — messenger molecules that draw inflammatory immune cells to the wound site. Their findings are groundbreaking: HPMN effectively reduced tissue inflammation by 50% and diminished wound size by an impressive 90% within just 14 days of treatment.
This pioneering approach offers a unique advantage over conventional treatments, which typically only manage surface inflammation. The HPMN's ability to clear harmful inflammatory factors from deep within the skin significantly enhances its potential for personalized wound care.
Looking Ahead: The Future of Wound Healing Technology
The advancements represented by SUC-MN and HPMN signify a monumental shift in wound healing methods and skin disease management. The NUS research team is keen to push these technologies into clinical settings, planning additional studies to further validate their effectiveness.
Future iterations of the extractive microneedles will incorporate controllable pore sizes using cutting-edge 3D printing and feature antibacterial properties essential for treating infections that frequently accompany non-healing wounds. The design of flexible microneedle patches is also in the pipeline to ensure optimal adhesion to various tissue types.
"We are thrilled about the transformative potential of our research and are eagerly anticipating bringing this technology to the clinical arena," stated Assistant Professor Tay. "These innovative approaches could provide significant relief not only for patients with diabetic wounds but also for individuals suffering from chronic skin conditions such as psoriasis and dermatitis."
In a world where diabetic wounds pose a rising threat, this groundbreaking research from NUS could mark a new era in effective and rapid wound healing solutions—offering hope to millions worldwide. Stay tuned, as we follow the exciting developments in this revolutionary technology!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)