Breakthrough in CAR T Cell Therapy: Engineered T Cells Overcome Resistance with Innovative Dual Vector System!
2024-12-24
Author: Rajesh
Introduction
In an exciting advancement for cancer treatment, researchers at City of Hope have unveiled a groundbreaking method that enhances the potency of CAR T cell therapy, a revolutionary treatment for specific blood cancers. This new system, detailed in a recent publication in Nature Biomedical Engineering, is designed to address a significant hurdle: the resistance that some patients develop against current CAR T cell therapies.
The Challenge of Tumor Resistance
CAR T cell therapy has been a beacon of hope for many battling cancer, allowing physicians to harness the body's immune system by reprogramming T cells to identify and attack cancer cells. However, the treatment is not foolproof, and certain tumors have developed mechanisms to evade detection by these engineered immune cells. "The tumor essentially becomes invisible to the T cells," explains Dr. Scott E. James, lead author of the study.
Innovative Dual Vector System
Traditionally, efforts to combat this resistance have focused on targeting individual strategies tumors employ to escape immunotherapy. However, capturing multiple escape routes has been a complex challenge due to limitations in the genetic information that can be delivered to T cells using current methods. Dr. James likens the problem to limited storage on a computer, where adding more storage via additional devices (in this case, a second vector) can effectively increase capacity.
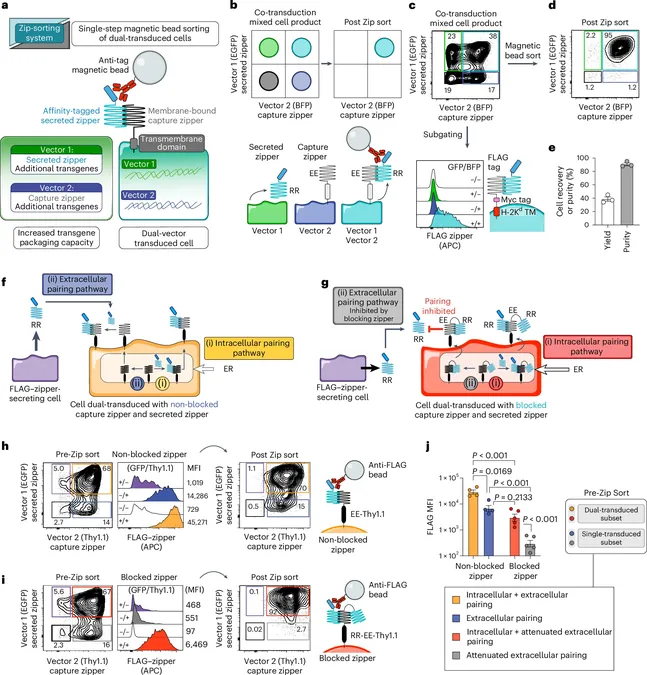
Enhanced Potency Through Zip-Sorting
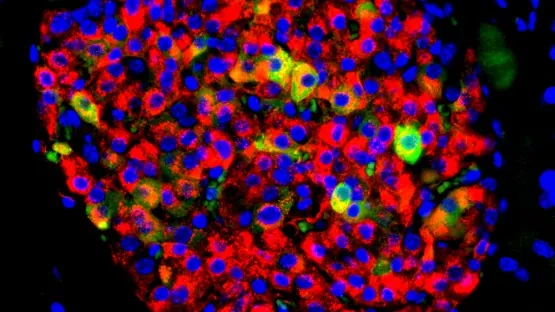
The researchers' innovative dual vector approach allows for the simultaneous targeting of multiple antigens—in this case, up to four—rather than the standard two. This method paves the way for T cells that can recognize various proteins found on cancer cells, increasing the likelihood of successful treatment outcomes.
Moreover, the new technique employs "switch receptors," which can convert negative signals from cancer cells into positive ones, mitigating T cell depletion and exhaustion, a common issue when T cells are persistently engaged with tumor cells. Tested with up to four different antigens and three switch receptors, this technique demonstrated enhanced anti-tumor activity, with T cells exhibiting prolonged survival and increased proliferation.
Collaboration and Future Directions
Collaborating with prestigious institutions like Memorial Sloan Kettering Cancer Center and the National Institutes of Health, Dr. James and his team engineered a sophisticated system now termed "zip-sorting." This method allows researchers to significantly increase the genetic complexity of engineered T cells, providing a powerful platform for constructing cellular therapies that can respond to multiple tumor targets while also resisting immune suppression.
Clinical Implications
While the current findings have been evaluated in mouse models, researchers are now gearing up for clinical implications. Optimizing zip-sorting for human applications could lead to advanced trials to determine the most effective combinations of switch receptors and CAR targets.
Revolutionizing Cancer Treatment
In addition to enhancing CAR T cell capabilities, the zip-sorting technology has the potential to revolutionize the field further by incorporating transcription factors that could improve T cell proliferation or implementing safety switches to deactivate T cells should they become overly aggressive.
“With these capabilities, we are on the brink of a new era in CAR T cell therapy, one where engineered T cells can confront multiple immune evasion strategies simultaneously,” Dr. James shares. This promising direction could not only improve outcomes for current cancer therapies but also inspire future innovations that enhance their effectiveness.
Conclusion
As scientists continue to unveil the intricacies of cancer treatment, the zip-sorting advancement stands out as a beacon of hope for many patients. The journey towards more robust and adaptive therapies is just beginning, and the potential to reshape cancer care is unprecedented!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)