Breaking Down the Barriers: Enhancing Physical Activity in Children and Adolescents with Congenital Heart Disease
2025-03-28
Author: Rajesh
Congenital heart disease (CHD) stands as the most common type of birth defect, impacting approximately 1% of newborns globally. In the United States alone, with a birth rate of nearly 3.6 million in 2023, this translates to around 360,000 infants potentially diagnosed with CHD. While nearly 97% of these children survive into adulthood due to advancements in medical technology, many face lifelong health challenges compounded by comorbid conditions. These realities underscore the urgent need for effective interventions aimed at enhancing physical activity and overall health in this vulnerable population.
The Crucial Role of Physical Activity
For years, healthcare providers remained skeptical about recommending physical activity to children with CHD due to concerns over safety. However, recent research contradicts previous fears, indicating that not only is regular physical activity safe for these patients, but it is also essential for improving cardiovascular health and reducing the prevalence of obesity, diabetes, and even enhancing mental well-being. Alarmingly, only 8% of children and adolescents with CHD meet the recommended standards of 60 minutes of daily moderate to vigorous physical activity. This alarming statistic highlights the pressing need to address barriers preventing these young patients from engaging in physical activities.
Unveiling Barriers and Facilitators
A comprehensive review has illuminated a spectrum of barriers that hinder physical activity among children and adolescents with CHD. These include:
1. Individual Factors
Psychological challenges, such as fear or anxiety about exertion, alongside feelings of inadequacy compared to peers, can severely limit engagement in physical activities. Conversely, self-efficacy plays a significant role in fostering participation, where the belief in one’s abilities is pivotal to overcoming these mental hurdles.
2. Social Influences
Family dynamics can both aid and obstruct physical activity. While supportive parents can encourage their children to be active, excessive worry from caregivers can restrict activity levels. School environments also play a crucial role; teachers’ perceptions about risk associated with CHD may inadvertently limit opportunities for physical engagement.
3. Socioeconomic Constraints
Financial barriers, such as costs associated with sports activities and lack of access to suitable environments, further exacerbate the situation. Many families are unable to afford the equipment or transportation necessary for active participation.
4. Environmental Factors
Inadequate facilities and harsh weather conditions can deter physical activity. Seasonal changes significantly affect participation levels, with extreme temperatures and the availability of safe, accessible spaces reported as major barriers.
Leveraging the COM-B Model for Change
By applying the COM-B model, an implementation framework in public health, researchers have successfully categorized the factors influencing physical activity into capabilities, opportunities, and motivations. This model establishes a foundation for developing targeted interventions aimed at enhancing physical activity for individuals with CHD, focusing on enhancing both environmental opportunities and individual motivations to embrace active lifestyles.
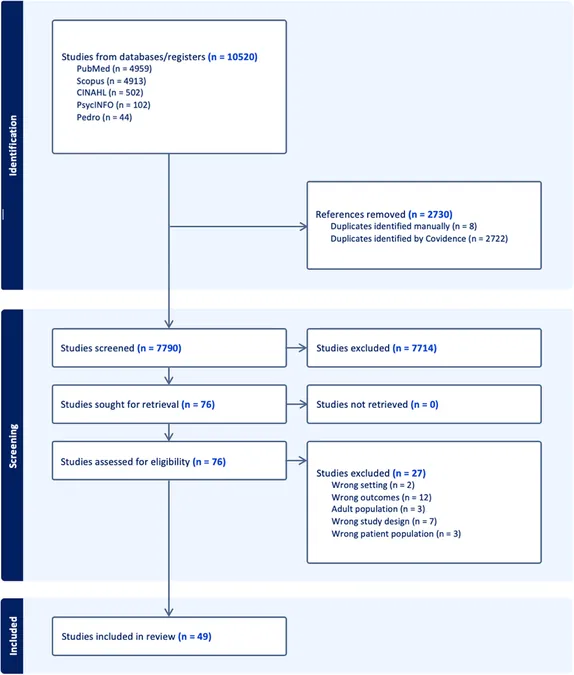
Global Perspectives on Research
With 49 studies reviewed from various countries, including leading research hubs like Canada and the United States, this review underscores the widespread implications surrounding the topic. However, it also reveals a gap in literature concerning low to medium quality evidence found in some studies. Future research efforts should focus on addressing these quality issues while exploring effective interventions through systematic approaches that consider the unique challenges faced by young patients with CHD.
Moving Forward: The Path to Improved Physical Activity
In response to the findings, the development of comprehensive educational programs for healthcare providers is urgent. These programs should focus on providing tailored guidance for children with CHD, fostering environments that encourage physical activity while alleviating parental fears. Furthermore, collaborative efforts between families, schools, and healthcare practitioners can create supportive networks that empower these young individuals to embrace active lifestyles confidently.
Conclusion
As CHD survival rates continue to improve, the emphasis on quality of life through physical activity becomes paramount. By addressing the multifaceted barriers affecting exercise in children and adolescents with CHD, we can enhance health outcomes and ensure these young patients lead fulfilling, active lives. It's time for a shift in perspective—let’s transform barriers into facilitators for the future of children with congenital heart disease!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)