Unveiling the Hidden Truth: Cancer Rates in UK Biobank Participants vs. General Population
2025-03-26
Author: Emma
Introduction
The UK Biobank stands as a prominent health resource globally, bringing together approximately 500,000 participants from 2006 to 2010. This extensive study has linked health records to national cancer and mortality registries, providing a treasure trove of data for medical and health research, particularly in cancer studies.
Concerns About Cancer Risk Models
Recent investigations have raised eyebrows regarding the reliability of cancer risk models developed using UK Biobank data, like those for prostate and breast cancers. A critical concern has surfaced: the cancer incidence among UK Biobank participants notably diverges from that of the general population. The accuracy of these models hinges on comparable cancer rates; discrepancies could skew the calibration results, leading researchers to misjudge the true risks of cancer.
Previous Studies on Cancer Rates
Before this, various studies found that cancer rates in UK Biobank participants are generally lower: men aged 70-74 showed an 11.8% decrease in incidence, and women 18.1% lower, alongside observed discrepancies in breast and colorectal cancers. However, prostate cancer rates appeared elevated. What remains unclear is whether similar inconsistencies extend to other types of cancer and how they may evolve over longer follow-up periods.
Recent Comprehensive Study
In a breakthrough comprehensive study, researchers aimed to juxtapose cancer incidences between UK Biobank participants and the general population, involving a comparison across 25 specific cancer types and assessing variances by demographics and socio-economic factors. A staggering 9.2 million NHS individuals residing within 25 miles of assessment centers were invited, leading to the eventual recruitment of over 502,000 participants, a mere 5.5% of those contacted.
Health Assessments and Data Collection
Participants underwent rigorous health assessments—questionnaires, interviews, and various sample collections—ensuring comprehensive insights into their lifestyle choices and health status. From the initial pool, they excluded individuals with prior cancer diagnoses or withdrawals, yielding a robust group of 466,163 participants.
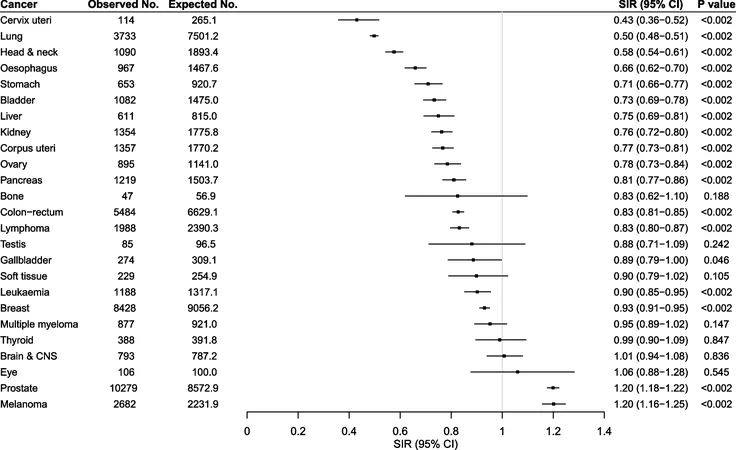
Diagnosis and Statistical Analysis
To diagnose cancer accurately, researchers relied on self-reported data and linked national cancer registries, covering various cancers including breast, prostate, lung, and more. The statistical analysis followed, focused on understanding how observed cancer incidences compared against expected figures based on population averages.
Findings of the Study
Findings revealed a sobering reality: cancer incidences among UK Biobank participants were, on average, 10% lower than expected. Higher incidences were recorded for specific cancers such as prostate and melanoma, attributed to health-conscious behaviors and proactive health checks among participants. Conversely, cancers like cervical and oesophageal were significantly less prevalent.
Patterns and Healthy Volunteer Bias
This research emphasized several striking patterns: older individuals exhibited a higher uniformity in cancer incidence, while common socio-economic factors influenced cancer risks across demographic lines. Alarmingly, it appeared that healthier lifestyles among UK Biobank participants may have bred a “healthy volunteer bias,” contributing to these findings.
Criticism and Implications for Future Research
Critics have raised concerns regarding the appropriateness of utilizing UK Biobank data for broad public health implications, suggesting that the observed cancer risks may not apply outside this study group. The implications are profound for cancer research and risk modeling, necessitating recalibrations to align findings with the general population.
Conclusion
In conclusion, while the UK Biobank remains a cornerstone of health research, the glaring discrepancies in cancer incidences signal a pressing need for a reevaluation of how data from this cohort is interpreted. As research continues to unfold, understanding these dynamics will be pivotal in crafting effective cancer prevention and treatment strategies.
Stay tuned as we continue to explore the consequences of these findings and their potential impact on future cancer research and healthcare initiatives.








 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)