
Unraveling the Mystery: How Just 3 Neurons Could Control Your Appetite!
2024-11-04
Author: Jacques
Unraveling the Mystery: How Just 3 Neurons Could Control Your Appetite!
Recent research on mice uncovers a remarkable simplicity behind the complex drive to eat—suggesting that merely three types of neurons in the brain may be responsible for influencing appetite. This groundbreaking study indicates that these neurons can either suppress or enhance the desire to eat, leading to significant fluctuations in food consumption.
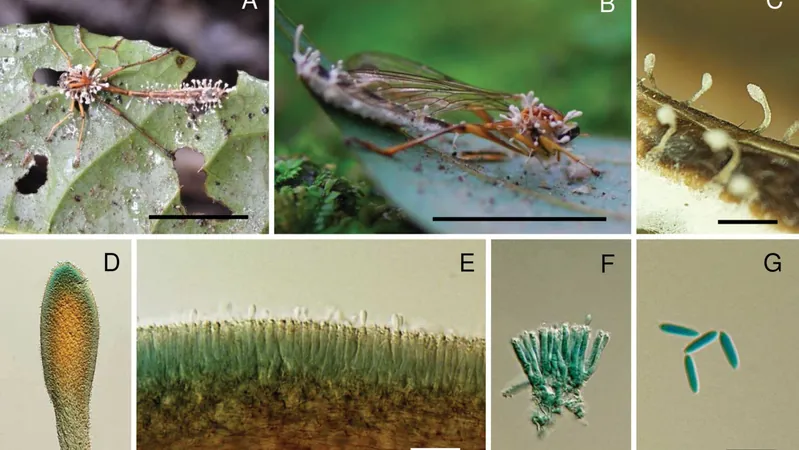
At the center of this intricate circuit are specialized neurons that detect crucial “hunger-signaling hormones.” These hormones inform the brain whether the organism is feeling full or hungry. Once activated, these neurons communicate with another set of neurons in a different brain region, which in turn influences a third group of neurons connected to the jaw. This final set of neurons orchestrates the necessary movements for chewing, creating a seamless reflex that often operates without conscious thought. Think of it as a reflex reaction akin to pulling your hand back from a hot surface—the hunger hormones act as the trigger, and chewing is the response.
Published on October 23 in *Nature*, this study draws attention to a circuit not only fundamental in mice but potentially in humans as well. If this neurobiological mechanism is confirmed in people, it could profoundly reshape our understanding of obesity. “The control of how much we eat and when we eat is not just about personal choice; it’s a fundamental circuit at work," explains Christin Kosse, the study's lead author and a research associate at The Rockefeller University in New York.
In light of this novel research, the growing acceptance of obesity as a chronic condition is more relevant than ever. Once considered merely a lifestyle choice, obesity is now recognized for its complex interplay of genetic, psychological, and physiological factors. This study reinforces the theory that innate biological differences could significantly influence eating behavior and weight management.
One of the critical concepts addressed in this study is known as “set point theory.” Research suggests that each person has a genetically predetermined weight range they naturally strive to maintain. Disruptions to the complex hormonal signals that typically trigger feelings of satiety after meals could potentially lead to overeating and consequent weight gain. For instance, after a satisfying meal, hormones released by fat cells and the gut alert the brain to halt eating, a process that can take about 20 minutes to kick in. If this signaling is disrupted, hunger can persist, leading individuals to consume excessive amounts of food, driving them toward obesity.
Past studies have highlighted that neurons in the hypothalamus—an area of the brain known to regulate appetite—are influenced by weight-loss drugs such as those classified alongside Ozempic. Notably, decreases in a protein known as brain-derived neurotrophic factor (BDNF) have also been linked to obesity in both animals and humans.
In their experiments, Kosse and her team found that BDNF-producing neurons in the hypothalamus were notably active in mice that became obese after a high-fat diet. This suggests a potential response where these neurons attempt to suppress appetite following weight gain. Remarkably, when researchers manipulated these neurons, the results were astonishing. Mice with suppressed BDNF neurons exhibited a staggering 1200% increase in food consumption, even displaying chewing motions without any food present, raising questions about automatic, reflexive eating behaviors.
On the flip side, when the BDNF neurons were activated, the mice significantly reduced their food intake and ceased chewing motions altogether. This vital finding presents the BDNF neurons as a critical switch in the brain’s hunger circuit. Kosse posits that similar neuronal systems likely exist in humans, which could revolutionize our approach to obesity management and treatment strategies.
Looking ahead, researchers are eager to delve deeper into how this neuronal circuit might fluctuate under various emotional states, such as anxiety, potentially unveiling more about the complex relationship between emotions and eating behavior. With this new knowledge, the narrative around obesity and appetite control could shift dramatically, opening new avenues for research and therapeutic intervention.
Stay tuned, as we unpack more exciting developments in the world of neuroscience that could change how we perceive our relationship with food forever!







 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)