
The Political Battle Over Disease Tracking: A Crucial Element of Public Health
2025-03-11
Author: Charlotte
The Political Battle Over Disease Tracking: A Crucial Element of Public Health
Efforts to monitor public health through essential datasets have faced increasing challenges, particularly since the onset of political shifts in 2025. Under executive orders from then-President Donald Trump, notable federal datasets—including the Centers for Disease Control and Prevention’s (CDC) Youth Risk Behavior Survey and various crucial HIV/AIDS data—were shielded from public access. This decision has raised concerns about transparency in health tracking, which is essential for managing diseases and protecting vulnerable communities.
Historically, the collection of public health data has never been a straightforward, politically neutral process. Rather, it has always intertwined concepts of individual rights and government responsibility. With insights from public health historians and ethicists, we recognize that surveillance remains a foundational tool in combating diseases and driving health policies.
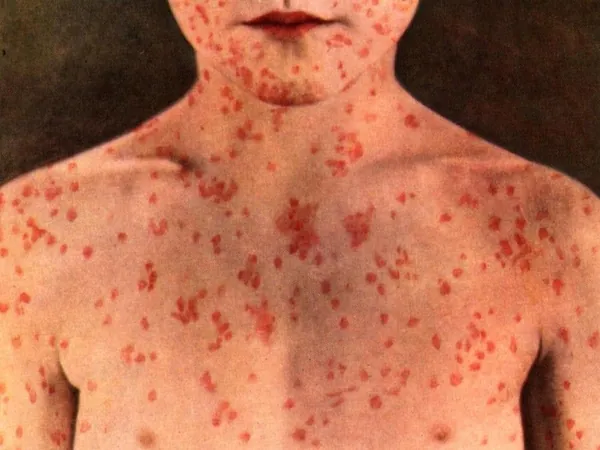
Surveillance involves tracking diseases among individuals to enable timely interventions such as isolation, quarantine, and treatment. This practice allows health officials to respond to environmental threats and efficiently allocate resources to areas and populations at heightened risk. By the early 20th century, public health advocates famously argued that without surveillance, efforts to control disease would be akin to "hunting birds by shooting into every green bush."
Three pivotal controversies in public health history illustrate the stakes involved in data collection:
1. Tuberculosis: The Fight to Share Names
The framework for disease surveillance was largely shaped by tuberculosis (TB) responses in the late 19th century, particularly as TB transitioned from a "disease of the elite" to a widespread affliction affecting the urban poor. New York City pioneered mandatory TB reporting, sparking considerable pushback from the medical community. Physicians argued this monitoring posed a threat to the doctor-patient relationship. However, the surveillance proved vital for reaching marginalized populations, ensuring they received the necessary care without public backlash overshadowing its importance.
2. HIV/AIDS: The Quest for Privacy
The emergence of the AIDS epidemic during Ronald Reagan's presidency brought heightened resistance to disease surveillance. Testing for HIV became available in the mid-1980s, igniting fears over privacy and discrimination among affected individuals. Gay rights activists, prioritizing confidentiality, campaigned against a national HIV registry, fearing it would lead to systemic discrimination. This struggle highlighted the tension between public health needs and the rights of individuals. Over time, effective treatment options led to a gradual acceptance of mandatory reporting.
3. Cancer: The Call for Accountability
Cancer surveillance, in contrast to TB and HIV, faced significant delays, driven by growing public concern over environmental factors. Activists, particularly mothers advocating for their children's health, demanded more accountability regarding cancer's spread, catalyzed by the National Cancer Act of 1971. Federal legislation eventually mandated cancer data collection, but it was not until 2000 that every state established cancer registries, reflecting communities' growing insistence on being counted.
The overarching lesson is that while public health surveillance has prompted resistance, communities often recognize its value as a protective mechanism. Nonetheless, it remains evident that the U.S. public health surveillance system is inadequately funded and piecemeal. The Pew Environmental Health Commission criticized birth defects surveillance as “woefully inadequate,” and persistent gaps in monitoring occupational diseases highlight the systemic issues that persist, making it "a century behind" in crucial areas.
Currently, the political implications of the Trump administration's changes to federal data systems are unfolding. Following a court order, some important public health datasets were restored, though they now come with disclaimers that reflect political rather than scientific perspectives. This situation underscores the ongoing struggle between the necessity for transparent health data collection and the influence of political ideologies—an issue of paramount importance for society as health crises inevitably arise.
As we navigate these complex dynamics, it is crucial to remember that robust disease tracking is not merely a bureaucratic obligation; it is a fundamental requirement for protecting public health and ensuring equitable access to medical resources for all individuals.








 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)