
Revolutionizing Juvenile Arthritis Diagnosis: The Promising Role of Ultrasound and AI
2025-04-03
Author: Charlotte
Juvenile arthritis, specifically juvenile idiopathic arthritis (JIA), is the most common rheumatic condition affecting children, impacting up to 25,000 young Canadians. Notably, the temporomandibular joints (TMJ), crucial for biting, chewing, and speaking, are often among the first—and sometimes the only—joints to show signs of the disease. This poses a pressing need for early diagnosis, as a delay may result in chronic pain, reduced mobility, and even permanent facial deformities.
In light of this, a dedicated research team at the University of Alberta is at the forefront of developing a more effective, safer, and cost-effective diagnostic method. By integrating portable ultrasound technology with artificial intelligence (AI), they aim to streamline the detection process, enhancing the screening capabilities for TMJ arthritis among children.
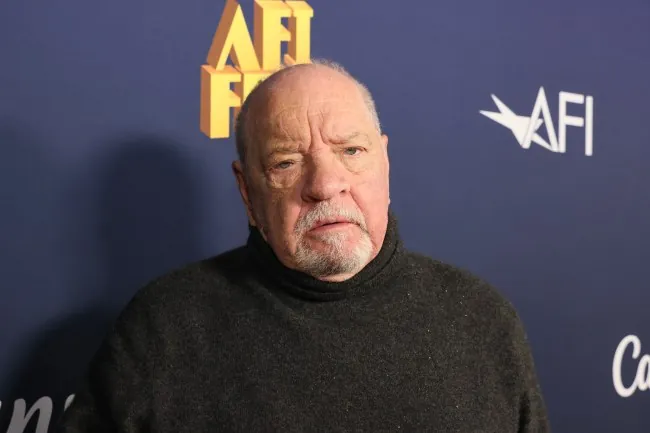
Current diagnostic techniques for TMJ arthritis present significant drawbacks. Cone-beam computed tomography (CBCT) exposes patients to radiation, while magnetic resonance imaging (MRI) is often prohibitively expensive, time-consuming, and sometimes necessitates sedation for pediatric patients. In stark contrast, ultrasound is a radiation-free, more affordable alternative. Principal investigator Fabiana T. Almeida, an assistant professor of oral and maxillofacial radiology, underscores this advantage: “Ultrasound has no radiation and is portable, but it’s challenging to interpret. That’s where AI comes in—to refine both the imaging and interpretation processes.”
Almeida leads a multidisciplinary team including radiologists, pediatric rheumatologists, and biomedical engineers from the University of Alberta and the University of Calgary. They are focused on assessing the effectiveness of hand-held ultrasound technology in detecting TMJ arthritis, exploring AI’s potential to generate 3D images—an innovation that could significantly enhance diagnostic accuracy. The goal is to expedite referrals to pediatric rheumatologists for further evaluation and confirmation of diagnosis using MRI.
Intriguingly, although ultrasound has not been widely utilized in a dental context historically, Almeida has pioneered its application for the last eight years, collaborating with ultrasound experts to innovate in this space. Previous studies have already laid groundwork for success in this project, as she developed an AI-driven image segmentation process that can improve clarity in joint imaging.
“Undiagnosed TMJ arthritis can severely hinder a child’s ability to bite properly and can even lead to complications such as sleep apnea,” warns Almeida. “Our research is fundamentally about improving early detection and ultimately enhancing the quality of life for affected children.”
Almeida's work is part of the larger Alberta Innovates LevMax-Health initiative, which recently allocated $9.9 million to support health innovations within the province. This initiative encompasses various projects, including those aimed at improving caregiver support and developing preventive strategies for neonatal ventilator-associated pneumonia.
As this research progresses, it represents a beacon of hope for early diagnosis and effective intervention, potentially transforming the landscape of juvenile arthritis care. The integration of advanced technology like AI with traditional medical practices could be the breakthrough that changes countless children’s lives for the better. Stay tuned as this story unfolds—it’s one that could redefine pediatric healthcare!







 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)