Groundbreaking Study Unravels 50-Year Mystery of Stem Cell Transplants: Is Donor Age the Key to Success?
2024-11-04
Author: Benjamin
Groundbreaking Study Unravels 50-Year Mystery of Stem Cell Transplants: Is Donor Age the Key to Success?
In an astonishing breakthrough, researchers from the Wellcome Sanger Institute and the University of Zurich have finally solved a 50-year enigma surrounding stem cell transplants: how does donor age influence the long-term success of these life-saving procedures? This pivotal study, published in the esteemed journal Nature, illuminates the cellular behavior of transplanted stem cells, providing crucial insights that could enhance donor selection and ultimately improve patient outcomes.
Understanding Stem Cell Transplants: A Lifeline for Patients
Stem cell transplants, also referred to as bone marrow transplants, are critical treatments for severe blood disorders, including life-threatening cancers such as leukemia and lymphoma. Every year, over a million people across the globe are diagnosed with blood cancer, and for many, a stem cell transplant could be their last chance for a curative treatment. In the United States alone, more than 22,000 hematopoietic cell transplants were conducted in 2021.
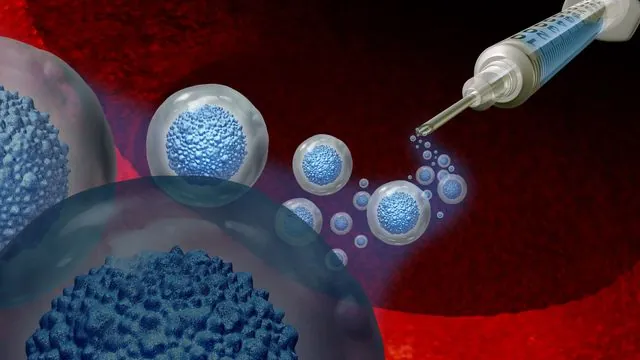
The transplant process begins with the patient undergoing chemotherapy or radiation therapy to eradicate the diseased cells within their bone marrow. Subsequently, healthy hematopoietic stem cells from a compatible donor are infused into the patient’s bloodstream. If the procedure is successful, these stem cells migrate to the bone marrow and commence the complex task of regenerating the blood and immune system—essentially rebooting the patient's biological machinery.
Despite the efficacy of stem cell transplants, their outcomes have historically varied widely. Factors such as donor compatibility, individual health conditions, and notably, donor age—all play significant roles in the complexity and success of these high-stakes procedures. Until now, our understanding of how transplanted cells behave over an extended period was limited, but Dr. Michael Spencer Chapman, director of health informatics at the Wellcome Sanger Institute, and his research team are shedding light on this vital area.
Revolutionary Findings on Donor Age and Transplant Success
The researchers meticulously analyzed genomic sequences from more than 2,800 blood samples sourced from 10 pairs of donor-recipient siblings, tracking cellular behavior from 9 to 31 years after transplant. Their findings were groundbreaking: transplants originating from younger donors (ages 18-47) saw up to 30,000 stem cells successfully engraft long-term, contributing significantly to blood production. In stark contrast, those from older donors (ages 50-66) only yielded between 1,000 and 3,000 stem cells that survived and maintained functionality, demonstrating a tenfold reduction in success rates.
The engrafted stem cells displayed the ability to generate a variety of blood cell types, including crucial myeloid cells and immune-supporting B and T lymphocytes. However, the research also flagged a tendency of certain individual clones to favor one type of mature blood cell, raising questions about the adaptability of the immune system post-transplant. Additionally, the study found that these transplanted stem cells exhibited accelerated aging in clonal diversity, with 10 to 15 years of maturity lost compared to the cells from the original donor—a stark reminder that age carries weight in cellular vitality.
The researchers mapped essential somatic mutations and epigenetic modifications in the survived transplanted cells that reflect the selection pressures encountered after transplant. This innovative approach pinpointed the genetic pathways that may enhance both the diversity and resilience of the transplanted cells, providing a roadmap for future improvements in patient outcomes.
A Glimpse into the Future of Stem Cell Transplantation
“Tracing decades of changes in a single sample has revealed how some cell populations emerge while others recede, fundamentally shaping the patient’s blood over time. It’s thrilling to gain such a detailed understanding of this process,” said Chapman. His team envisions further exploring additional factors influencing long-term hematopoietic stem cell dynamics, aiming to tailor both donor selection and the pre-transplant conditioning landscape for optimal stem cell function.
Dr. Markus Manz, a senior author and director of medical oncology at the University of Zurich, echoed this sentiment. “Our findings underscore that age is more than just a chronological measure; it significantly impacts transplant success rates. Identifying genes that exhibit somatic mutations or epigenetic changes at various stages of transplantation may hold the key to dramatically improving this life-saving procedure.”
These compelling discoveries also underscore a pivotal shift in donor demographics. The charity Anthony Nolan has responded by lowering the age of recruitment for their stem cell register to 16, promoting awareness of the potential for younger donors to provide better outcomes for patients requiring unrelated transplants.
With this revolutionary research, the future of stem cell transplantation looks brighter than ever. The next steps involve discovering the genes that might enable certain stem cells to thrive better than others, potentially leading to groundbreaking advancements in the field and an increase in successful transplant procedures worldwide.
Stay tuned as this story develops, as scientists continue to peel back the layers of complexity surrounding stem cell transplants, unlocking new possibilities for patients in need of hope and healing.









 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)