Groundbreaking Study Aims to Uncover the Link Between Delirium and Dementia in Mild Cognitive Impairment Patients
2024-11-07
Author: Jacques
Background
Delirium, an acute disturbance characterized by confusion, memory issues, and altered consciousness, is a pressing concern among older adults, particularly those with chronic health conditions. Shockingly, up to 55% of hospitalized elderly patients experience delirium, leading to numerous negative outcomes, including prolonged hospital stays, increased caregiving burdens, and higher mortality rates.
Alarmingly, existing mild cognitive impairment (MCI) not only serves as a major risk factor for delirium but also increases the likelihood of dementia development. Currently, the global prevalence of dementia is estimated at 5-7%, a figure projected to triple in the next two decades, alongside soaring medical costs that could reach $818 billion annually.
MCI, which affects approximately 6.7-25.2% of older adults, is often viewed as a precursor to dementia. The conversion rate from MCI to dementia within this demographic is alarmingly high at 10-15%, in stark contrast to the general population's conversion rate of just 1-2%. Moreover, those with MCI undergoing surgery may face an even higher rate of postoperative delirium, complicating their medical trajectory.
Despite some existing research, there is a glaring lack of studies exploring the long-term effects of delirium on the conversion of MCI to dementia. This underscores the urgent need for proactive measures against delirium, highlighting its prevention as the most viable strategy for mitigating the risk of dementia.
Objective
The primary goal of the proposed three-year study conducted in Korean long-term care hospitals is to delve deep into the incidence of delirium in MCI patients and its subsequent effects on dementia conversion. Additionally, researchers aim to create an advanced AI algorithm capable of predicting the transition from MCI to dementia based on gathered data. Key areas of focus include: 1. Analyzing the incidence and outcomes of delirium within MCI patients. 2. Investigating the relationship between delirium onset and the conversion rate to dementia. 3. Developing a reliable AI tool to assist in early prediction of dementia progression.
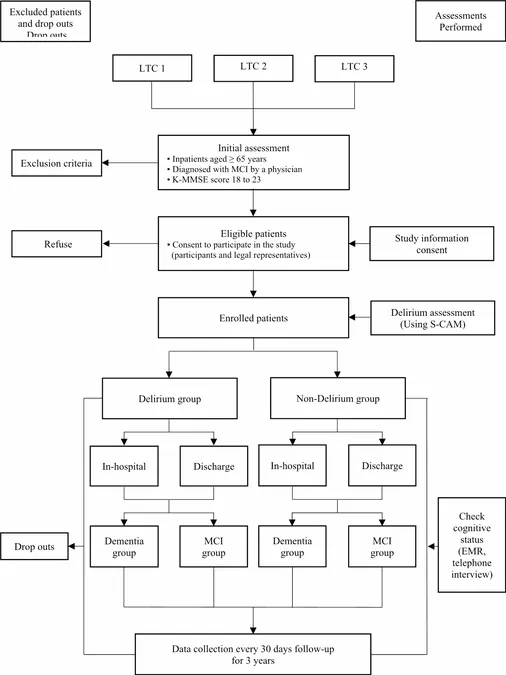
Study Design
This multicenter prospective cohort study consists of two parallel groups, adhering to the STROBE guidelines to ensure robust observational reporting. The first year focuses on establishing a standardized cohort by recruiting eligible patients, while the following years will facilitate ongoing assessments and the development of a web-based application for data analysis.
Participants will be monitored at 30-day intervals to gather critical data on delirium prevalence, survival rates, and conversion rates to dementia over a period of three years.
Participant Eligibility and Recruitment
Participants aged 65 and older, diagnosed with MCI, will be recruited from three major long-term care facilities in Korea. Only those with consent from their legal guardians will be included to ensure ethical standards are met. Inclusion criteria focus on cognitive assessments, while individuals with severe conditions or unable to provide consent will be excluded.
Data Collection and Analysis
Researchers will meticulously monitor a variety of characteristics and variables related to participants' health and living conditions, which could influence both delirium and dementia risk. Tools like electronic medical records and validated assessments will provide a comprehensive view of participants' health statuses.
The prevalence of delirium within the MCI cohort will be analyzed, taking into account associated risk factors and outcomes over time to aid in understanding how delirium impacts dementia development.
Outcomes and Significance
Among the key outcomes will be the assessment of the prevalence of delirium in MCI patients, mortality rates, hospital stay durations, and treatment costs incurred during hospitalization.
This ambitious study not only seeks to highlight the need for early interventions in at-risk populations but also aims to equip medical professionals with tools to better identify and manage cognitive decline. By bridging the gap between delirium and dementia, researchers hope to initiate a paradigm shift in how these conditions are understood and treated, ultimately lessening the socio-economic burden on healthcare systems worldwide.
Limitations and Future Directions
Despite its potential, the study anticipates challenges such as managing patient follow-ups and the impact of external factors, such as hospital visitation restrictions due to COVID-19. Nonetheless, the insights gleaned from this research will be invaluable in shaping future strategies for dementia prevention and care.
As our understanding of delirium's role in cognitive decline expands, so too does the hope for improved patient outcomes and reduced healthcare costs. The findings could redefine clinical practices and empower caregivers and healthcare providers with knowledge that leads to better patient care.
Stay tuned for more updates as this groundbreaking study unfolds, potentially transforming the future of dementia research!








 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)