Groundbreaking Discovery Could Revolutionize Treatment for Drug-Resistant Leukemia Patients!
2024-11-07
Author: Emma
Groundbreaking Discovery Could Revolutionize Treatment for Drug-Resistant Leukemia Patients!
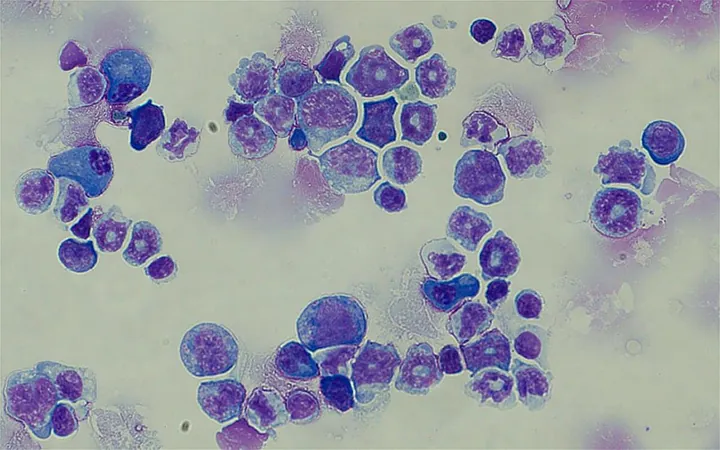
In a significant advancement in the fight against chronic myeloid leukemia (CML), researchers from Duke-NUS Medical School and their collaborators have uncovered a genetic variation that may explain the drug resistance seen in many patients, particularly among East Asian populations. This fascinating discovery highlights the urgent need for precision therapy in the face of a growing cancer crisis.
The Genetic Culprit: MCL-1 and BIM Variation
The study, published in the prestigious journal Leukemia, pinpoints an inherited genetic variation that plays a crucial role in enabling cancer cells to resist conventional leukemias treatments. Specifically, around 12 to 15% of individuals of East Asian descent carry a variation in the gene responsible for producing a protein known as BIM (BCL-2 interacting mediator of cell death). This protein is essential for inducing cell death in damaged or unwanted cells—a process many cancer treatments rely upon.
As cancers evolve, they often develop escape mechanisms to survive despite treatment pressures. The research team identified that this genetic variation alters BIM, allowing leukemia cells to thrive even when treated with common tyrosine kinase inhibitors like imatinib—a frontline therapy that typically helps eliminate cancerous cells.
From Discovery to Therapy: A New Weapon Against CML
The implications of this research are promising. By inhibiting the activity of a related protein called MCL-1, scientists demonstrated in lab studies that they could effectively target and kill these otherwise resistant cancer cells. Dr. Giselle Nah, a leading author of the study, emphasized the importance of understanding the relationship between genetic variations and treatment efficacy, stating, "Our findings indicate that leukemia cells carrying the BIM variation exhibit a biological advantage—namely, greater resistance to conventional apoptosis."
By utilizing a specially designed pre-clinical model, the research team further investigated this relationship, leading to targeted therapies that combine MCL-1 blockade with existing treatments, significantly enhancing their effectiveness.
Hope for Thousands: A Game-Changer for Patients
Professor Ong Sin Tiong, a senior study author, heralded this groundbreaking approach as a beacon of hope for patients battling drug-resistant forms of leukemia. "Targeting MCL-1 could potentially reduce disease progression in CML patients whose cancer cells are bolstered by genetic variations. This could herald a new era of cancer treatment where therapies are tailored to the genetic make-up of each patient," he explained.
The study's findings resonate beyond just leukemia. Researchers are now looking at the broader implications this knowledge could hold for other cancer types, such as certain lung cancers, which also employ similar mechanisms to evade treatment.
As an acknowledgment of the study's significance, Duke-NUS Associate Professor Charles Chuah emphasized the importance of genetic testing in diagnosing cancer. "Identifying patients who may carry the BIM variation at the onset of their diagnosis allows for early intervention with more aggressive therapies—a critical step in improving both survival rates and quality of life for patients in the East Asian population."
This pioneering research exemplifies how modern science is moving towards a more personalized approach in treating complex diseases like cancer, offering a glimmer of hope to countless patients and their families. As the scientific community continues its quest for precision medicine, the journey towards effective treatments becomes brighter, paving the way for revolutionary breakthroughs in cancer therapy.





 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)