Unveiling the Secret Power of Physical Forces in Cancer Immunotherapy
2024-11-07
Author: Siti
Introduction
A groundbreaking study from researchers at Georgia Tech and Emory University has illuminated the complex relationship between physical force and the efficiency of cancer immunotherapy, particularly focusing on the programmed cell death-1 (PD-1) pathway. Known for its crucial role in checkpoint inhibitors, PD-1 is a key player in how the immune system recognizes and combats cancer cells.
Role of PD-1 in the Immune System
In a healthy body, PD-1 acts as a gatekeeper, a receptor protein situated on the surface of T cells. Its main role is to bind with ligands, namely PD-L1 or PD-L2, from neighboring cells. This binding triggers a signal that instructs T cells to refrain from attacking healthy tissues. However, cancer cells can also masquerade themselves by producing ligands that bind to PD-1, tricking the immune response into inaction during critical moments.
Checkpoint Inhibitors and Their Limitations
Checkpoint inhibitors aim to block the interaction between PD-1 and these ligands, empowering T cells to fully engage in the fight against cancer. However, despite the promise of these therapies, it’s disheartening that only 20-40% of patients derive significant benefits from them.
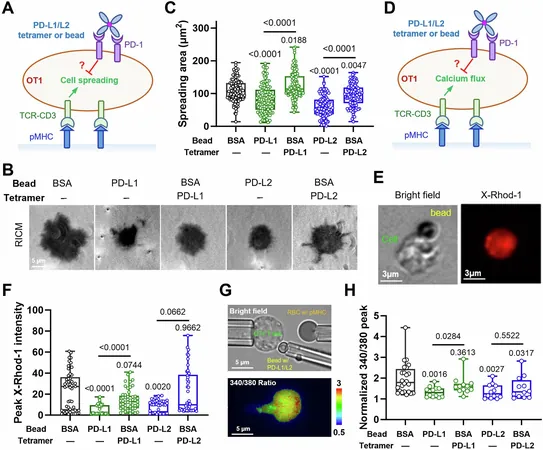
Investigating PD-1’s Mechanism of Action
One critical question has remained unanswered: what exactly drives PD-1 to issue a “stand-down” command to T cells? Interestingly, not all ligand binding leads to T cell suppression. The research team, led by Cheng Zhu from the Wallace H. Coulter Department of Biomedical Engineering, has identified mechanical force as a key contributing factor.
Role of Mechanical Forces in PD-1 Activation
“Mechanical forces are an important but previously overlooked component of immunology, especially regarding PD-1 activity,” Zhu stated. His team’s latest research, published in the journal *Nature Communications*, showcases that PD-1 activation is not merely about binding with ligands—it also requires an anchored surface that allows T cells to apply measurable forces.
Research Methodology
The researchers’ innovative approach involved molecular tension probes and biomembrane force probes to assess how T cells interact with PD-1 on cancer cells. Results indicated that T cells exerted forces ranging from 4.7 to 12 piconewtons. Intriguingly, when the applied force fell below 7 piconewtons, the interaction between PD-1 and the ligand strengthened and persisted longer; however, forces exceeding 8 piconewtons caused the bond to weaken and break.
Findings and Implications
“It's a delicate balancing act,” Zhu explained. “The right amount of physical force can dictate whether PD-1 inhibits or allows T cell action against cancer cells.
Moreover, Zhu’s team discovered that soluble PD-L1 ligands present in the bloodstream lacked the mechanical support necessary for PD-1 activation, therefore explaining why these ligands do not trigger T cell inhibition as effectively as those bound to a cellular surface.
Future Directions
The implications of this research are profound. It underscores the need for both physical and chemical signals in the regulation of PD-1 activity, revealing that even the slightest mechanical forces can influence the immune system's ability to fight cancer effectively.
Looking ahead, the team is eager to translate their lab findings into real-world applications by experimenting with animal models. This research not only promises to enhance our understanding of immune responses but also paves the way for more effective cancer therapies that could benefit a wider range of patients.
Conclusion
Stay tuned for further developments in this exciting area of cancer research and potential breakthroughs in immunotherapy that could change the landscape of treatment for millions.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)