Unveiling the Rare: A Deep Dive into Small Cell Neuroendocrine Carcinoma of the Ovary
2025-07-22
Author: Rajesh
Introduction to a Rare Diagnosis
Ovarian small cell neuroendocrine carcinoma (OSCNEC) is a puzzling and uncommon malignancy, with very few documented cases making its preoperative diagnosis quite challenging. Notably, the imaging characteristics of OSCNEC, especially those associated with positron emission tomography using fluorodeoxyglucose (FDG-PET), have yet to be explored in detail in published reports. This article presents a unique case study accompanied by a comprehensive review of the existing literature.
A Case Study That Shocked the Medical Community
Meet a 74-year-old woman whose journey began with troubling abdominal distension, leading her to our facility. She was sent over due to the identification of a pelvic mass via ultrasonography. Initial blood tests unveiled alarming levels of cancer markers—cancer antigen 125 was at 203.0 U/mL (normal: 0-35.0 U/mL) and neuron-specific enolase (NSE) was at 47.6 ng/mL (normal: 0-16.3 ng/mL).
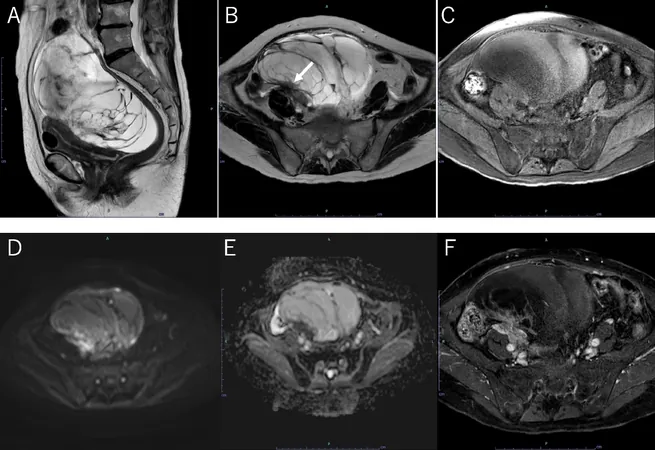
When magnetic resonance imaging (MRI) scans were performed at a high resolution of 3.0 Tesla, a multilocular cystic tumor, measuring 18 cm, was discovered. This mass exhibited irregular septa and featured a solid component that hinted at possible hemorrhage. Radiological evidence of peritoneal thickening and nodules indicative of dissemination was also observed.
PET/CT Reveals Disturbing Metastatic Spread
The situation escalated when FDG-PET/CT scans uncovered high levels of FDG uptake in the tumor's solid core, registering a maximum standardized uptake value (SUVmax) of 13.0. Further investigations unveiled metastases to the para-aortic lymph nodes, spine, iliac bones, and liver, along with peritoneal dissemination, leading the medical team to suspect intertrabecular bone metastases.
Surgical Intervention and Subsequent Findings
To clarify the situation, an extensive surgical approach was taken, involving bilateral salpingo-oophorectomy, omentectomy, and appendectomy. During the procedure, peritoneal dissemination was confirmed. The tumor, featuring a complex structure of irregular cysts and solid components, was confirmed to be a primary OSCNEC.
Decoding the Disease: Histological Findings
Microscopic examination revealed a distinct arrangement of the tumor cells, characterized by hyperchromatic nuclei and scant cytoplasm. Immunohistochemical analyses showed positivity for chromogranin and CD56, hinting at the neuroendocrine nature of the cancer. This diagnosis was pivotal as it also helped differentiate OSCNEC from other cancers such as small cell lung carcinoma.
Understanding the Implications of OSCNEC
Small cell cancers of the ovary represent a minuscule fraction of gynecological malignancies, primarily seen in postmenopausal women. The rarity of OSCNEC makes diagnostic criteria fluid, often relying on serum levels of NSE and imaging findings. The elevation of NSE, typically associated with neuroendocrine tumors, serves as an important diagnostic marker.
The Significance of Imaging and NSE Levels
Patients with OSCNEC often present elevated serum NSE levels, especially if metastases are present. The discovery of such metastases in our case underscores the importance of using FDG-PET imaging, which can provide critical insights not visible in other imaging modalities. It allows for a more complete preoperative staging, essential for better treatment planning.
Conclusion: A Wake-Up Call for Early Detection
Though OSCNEC remains a diagnostic enigma due to its indistinct imaging features, this case highlights that in the face of elevated NSE levels and specific patterns of metastasis, OSCNEC should remain a consideration among clinicians. The integration of comprehensive imaging techniques, alongside serum marker scrutiny, could vastly improve early detection and ultimately enhance patient outcomes. This case not only sheds light on a rare cancer type but also emphasizes the need for continued research and awareness in the medical community.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)