Unveiling the Malaria Crisis: A Decadal Look at Rwanda's Battle Against the Disease (2012-2022)
2024-09-16
Malaria, caused by Plasmodium parasites spread through the bites of infected Anopheles mosquitoes, remains one of the most daunting public health challenges globally. Despite a 37% drop in malaria incidence and 60% in mortality rates from 2000 to 2015 due to global health initiatives, nearly 249 million malaria cases were reported across 85 endemic countries in 2023, as highlighted in the World Malaria Report 2023 by the World Health Organization (WHO). Among the most afflicted nations, Nigeria, the Democratic Republic of the Congo, and Uganda led the grim statistics, accounting for a significant share of global malaria deaths, predominantly among children under five years old.
Rwanda's struggle with malaria dates back to the early 2000s, when the nation recorded over 5 million cases annually. However, concerted efforts from 2005 to 2012 led to an astonishing 86% reduction in incidence. Despite this notable progress, malaria transmission dynamics are constantly evolving due to various demographic, climatic, and public health factors.
In a bid to refine strategic planning and intervention, recent studies have been initiated to better understand the intricate patterns of malaria across Rwanda between 2012 and 2022. This research not only highlights the need for demographic-specific approaches but also pinpoints districts most at risk, enabling health officials to tailor public health interventions more effectively.
Rwanda’s geography, characterized by diverse landscapes and climates, significantly influences malaria transmission. The country’s elevation ranges between 1,500 to 2,000 meters above sea level, and with an annual average temperature of 18.5°C, it becomes a breeding ground for malaria-carrying mosquitoes during its two rainy seasons.
With a population exceeding 13 million, the majority residing in rural areas, understanding demographic distinctions is paramount. Vulnerable groups, including children, pregnant women, and the elderly, face varying susceptibility to malaria, necessitating targeted strategies. Public health improvements such as the distribution of long-lasting insecticidal nets (LLINs), indoor residual spraying (IRS), and larval source management (LSM) have been major components in reducing malaria transmission.
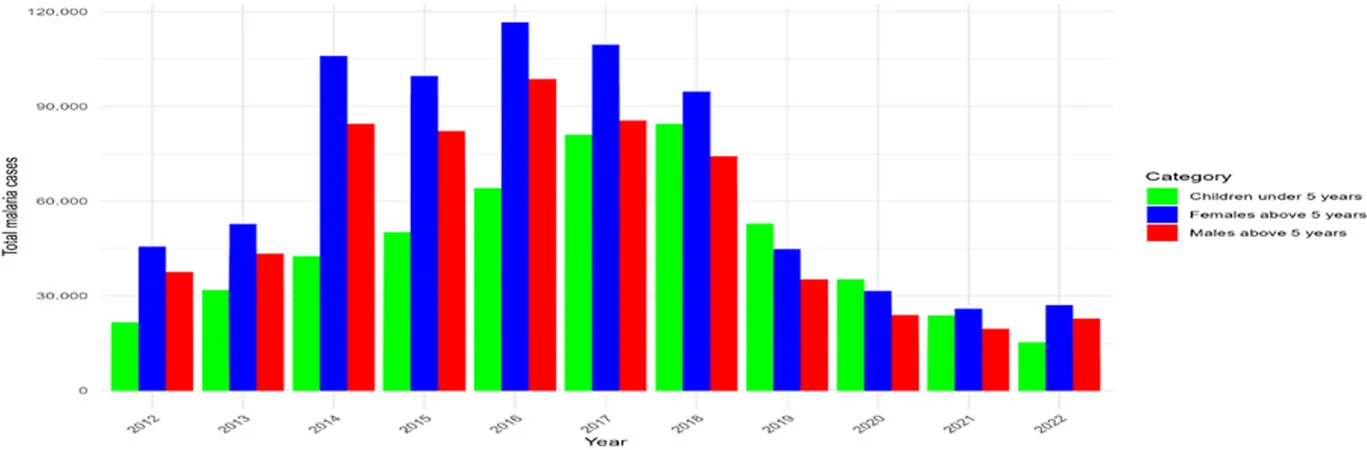
The spatio-temporal analysis from 2012 to 2022 revealed concerning trends: there was a spike in cases particularly among children under five years, with significant variances in incidence across districts. Notably, the district of Ngoma recorded alarmingly high incidence rates of 670.5 cases per 1,000 children, highlighting alarming disparities in malaria burden.
Clusters of high malaria incidence were identified in districts like Bugesera and Gasabo, with an observed-to-expected case ratio indicating alarmingly higher rates than anticipated. This geographical mapping of malaria cases emphasizes the need for localized interventions that address specific needs, enabling health authorities to allocate resources effectively.
Furthermore, data-driven insights obtained from regression models indicate that the elevated malaria risk is influenced by factors such as environmental conditions, socio-economic status, and healthcare access. The unveiling of these risk clusters calls for enhanced surveillance and adaptive public health policies tailored to the dynamics of malaria transmission.
In conclusion, the fight against malaria in Rwanda requires continuous, evidence-based efforts that evolve alongside the shifting landscape of disease transmission. The active exploration and implementation of targeted interventions aimed at high-risk demographic groups can pave the way toward significant reductions in malaria cases, fostering health equity and improving overall healthcare delivery across the nation. The proactive measures taken today will not only save lives but also help eliminate malaria as a public health threat in Rwanda for future generations.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)