Unveiling the Link: Immune-Inflammation Index and Inflammatory Bowel Disease Outcomes
2025-05-29
Author: Nur
Introduction: A Groundbreaking Meta-Analysis
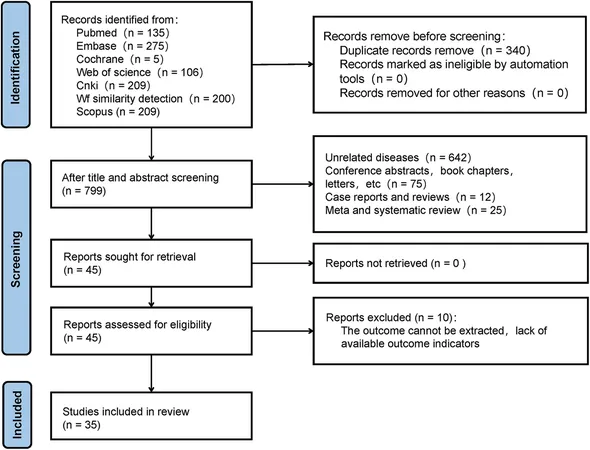
In a comprehensive exploration of inflammatory bowel disease (IBD), researchers conducted a systematic review and meta-analysis examining the connection between the immune-inflammation index and patients' clinical outcomes. This investigation analyzed 35 studies with a staggering total of 5,870 participants.
Study Selection and Quality
Out of an initial pool of 1,139 articles, many were eliminated due to duplicates and irrelevant content. Ultimately, 35 high-quality studies from various countries, including Turkey, China, and Japan, were included based on strict quality criteria.
Immune-Inflammation Indices: Understanding Their Roles
The analysis focused on several key indices: Neutrophil-to-Lymphocyte Ratio (NLR), Platelet-to-Lymphocyte Ratio (PLR), and Lymphocyte-to-Monocyte Ratio (LMR), alongside others like C-Reactive Protein/Albumin (CRP/ALB). These biomarkers were scrutinized for their ability to predict disease severity and activity in IBD patients.
Key Findings: NLR, PLR, and LMR
The results revealed that while NLR levels significantly increased in severe IBD cases, they did not predict severity categorically. Notably, high NLR correlated with heightened disease activity—suggesting it could be a reliable indicator for monitoring IBD progression.
In contrast, PLR emerged as a potent predictive marker, with increased levels observable in severe IBD cases, indicating its potential utility in clinical settings. Conversely, LMR's predictive capacity appeared inconsistent, raising questions about its reliability.
Pathophysiological Insights
The study delved into the mechanisms behind these biomarkers. It highlighted that neutrophils and lymphocytes play crucial roles in immune responses, with shifts in their ratios potentially reflecting inflammatory states associated with IBD.
Emerging Trends and Clinical Implications
As predictive biomarkers, NLR, PLR, and others could revolutionize IBD management, enabling healthcare providers to tailor treatments effectively based on individual inflammatory profiles. This approach emphasizes the growing importance of serum biomarkers in clinical decision-making.
Conclusion: A Path Forward in IBD Management
As the findings illuminate the intricate relationship between immune-inflammation indices and IBD outcomes, further investigations will be essential. Future research should extend beyond the current populations and explore these biomarkers' utility in diverse demographic settings. Ultimately, establishing robust predictive markers could enhance patient stratification and treatment guidance in the ongoing battle against IBD.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)