Unveiling the Impact of Sarcopenia Screening Tools in Preoperative Elderly Patients with Colorectal Cancer
2025-03-28
Author: Arjun
Colorectal cancer (CRC) emerges as the third most commonly diagnosed cancer globally and ranks second in cancer-related mortality. While prognostic evaluations in CRC typically hinge on clinical and pathological staging, other factors, particularly those related to patient physiology, significantly affect long-term survival rates and the likelihood of complications post-surgery.
Recent studies highlight the importance of body composition in assessing patient outcomes, particularly the influence of diminished skeletal muscle mass and increased visceral fat on survival. Sarcopenia, a condition involving the progressive loss of muscle mass and strength, particularly in elderly patients, is increasingly recognized for its adverse impact on surgical outcomes and overall prognosis in CRC. Alarmingly, recent statistics show that 37% of CRC patients may experience sarcopenia, amplifying their risk for postoperative complications and extended hospital stays.
Despite the critical role of sarcopenia in treatment outcomes, its assessment remains inconsistent in clinical practice. The European Working Group on Sarcopenia in Older People (EWGSOP2) and the Asian Working Group for Sarcopenia (AWGS) provide frameworks for diagnosing sarcopenia, which typically involves sophisticated imaging techniques and physical performance metrics. These diagnostic methods, though effective, often present practical challenges due to their cost and requirement for specialized personnel.
To better address these issues, the EWGSOP2 and AWGS recommend simplified screening tools such as SARC-F, SARC-CalF, and the Mini Sarcopenia Risk Assessment (MSRA). Each of these tools employs a mix of self-reported metrics and basic physical assessments to identify potential sarcopenia in patients. Notably, some screening tools have shown varied sensitivities and specificities, making the optimal choice for different clinical scenarios challenging.
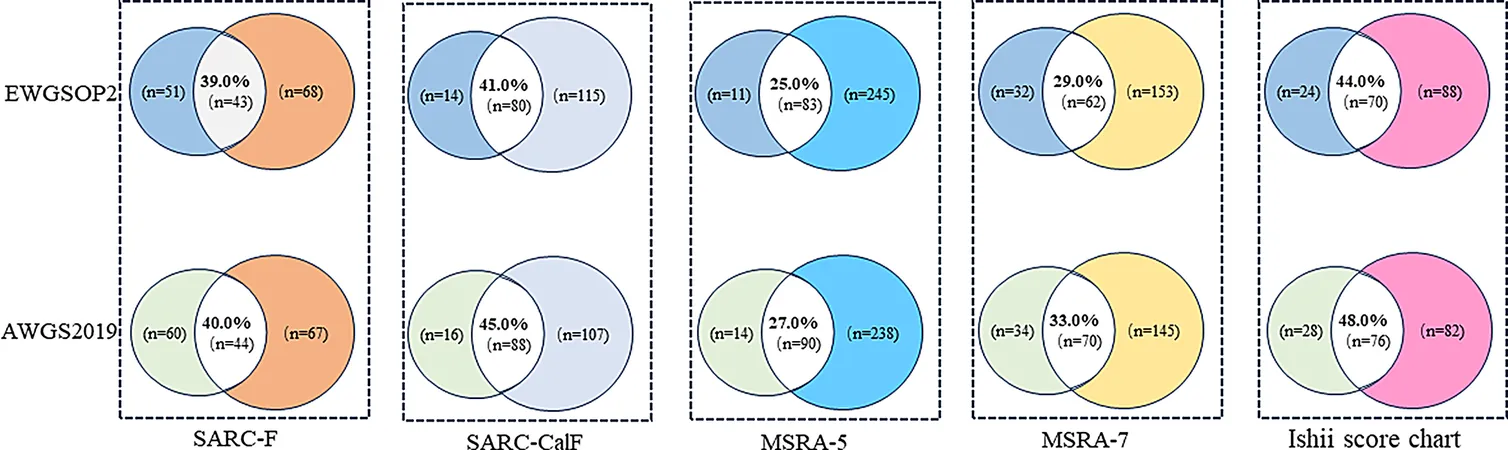
Our recent study, conducted at the Peoples Hospital of Wuxi city affiliated with Nanjing Medical University, sought to compare the effectiveness of various sarcopenia screening tools in elderly patients diagnosed with colorectal cancer who were preparing for surgery. We specifically investigated SARC-F, SARC-CalF, MSRA-5, MSRA-7, and the Ishii score in a cohort of 482 elderly patients, providing crucial insights into the prevalence and screening effectiveness of sarcopenia in this population.
Our findings revealed that using the EWGSOP2 criteria, 19.5% of participants met the criteria for risk of sarcopenia, while the AWGS2019 criteria identified 21.5%. However, the screening tools revealed a spectrum of results, with MSRA-5 indicating the highest risk at 68%.
During our analysis, the sensitivity and specificity of the screening tools varied significantly. Both SARC-CalF and the Ishii score chart emerged as strong contenders in accurately identifying sarcopenia, with the latter being particularly notable for its ability to exclude the presence of sarcopenia effectively.
Despite some limitations in our study, including reliance on bioelectrical impedance analysis rather than more robust imaging techniques, our findings underscore the urgent need for validated, accessible screening tools in clinical settings. The varied effectiveness of different screening tools in predicting sarcopenia risk reinforces the importance of customized approaches in managing elderly patients with colorectal cancer.
In conclusion, choosing the right sarcopenia screening tool could significantly impact treatment outcomes for elderly patients with colorectal cancer. A tailored approach in applying these screening methods may enhance early detection, inform intervention strategies, and ultimately improve patient prognoses, emphasizing the importance of integrating sarcopenia assessment into preoperative evaluations. As the healthcare system navigates the complexities of treating an aging population, these efforts to streamline and validate screening techniques will prove vital in advancing patient care.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)