Unveiling the Hidden Struggles of Borderline Personality Disorder in Inpatient Settings
2025-05-05
Author: Siti
The Toll of Borderline Personality Disorder (BPD) on Lives and Society
Borderline Personality Disorder (BPD) is more than just a diagnosis; it's a burden that affects individuals and society alike. Characterized by self-destructive impulsivity, emotional instability, and deep-seated issues with identity and relationships, BPD presents severe challenges. Research indicates that about 75% of individuals with BPD attempt suicide at least once, and roughly 10% tragically complete the act. This alarming statistic underlines the urgent need for effective intervention.
Surging Prevalence in Psychiatric Care
BPD's prevalence is strikingly high in psychiatric settings, with estimates suggesting it affects 12% of outpatient and up to 22% of inpatient individuals. Patients diagnosed with BPD often find themselves stuck in a revolving door of hospitalization without receiving the comprehensive, long-term care they desperately need. Many go undiagnosed despite showing clear symptoms, leaving them vulnerable and untreated.
Inpatient Hospitalization: A Double-Edged Sword
While inpatient care is typically not the ultimate solution for BPD, clinical guidelines suggest it can be a necessary step during acute crises, particularly when faced with suicidal tendencies or self-destructive behavior. Despite this, studies show that patients with BPD tend to experience distinct challenges during hospitalization, including higher rates of readmission compared to their peers.
The Need for Reliable Assessment Tools
A pressing need exists for validated screening instruments, like the McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD), to improve diagnosis and treatment of BPD within hospital settings. This instrument provides a straightforward approach for clinicians to assess BPD traits based on DSM-5 criteria, allowing for improved identification and care planning.
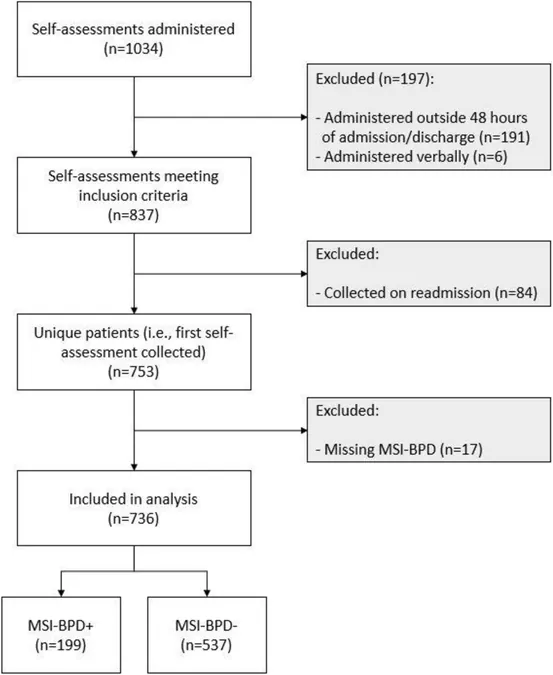
A Study in Numbers: Identifying BPD in Inpatients
A recent study conducted with 1,034 adults admitted to a specialized psychiatric unit revealed that around 26% screened positive for BPD traits. These individuals presented with significantly higher levels of distress, including depression and anxiety, compared to those without BPD features. The findings affirm the urgent need for accurate diagnosis to provide appropriate care.
Improvement in Symptoms: A Flicker of Hope?
Patients who screened positive for BPD showed noteworthy improvement in symptoms during their hospital stay. Specifically, these patients reported heightened anxiety and depression upon admission, yet many demonstrated substantial alleviation of their symptoms by discharge. This prompts questions about the effectiveness of short-term inpatient care in stabilizing BPD symptoms.
Addressing the Disconnect: Recommendations for Better Care
To enhance treatment outcomes for BPD patients, it's crucial to bridge the gap between acute care and effective long-term management. Recommendations include ensuring thorough assessments upon admission, providing psychoeducation about BPD, and securing appropriate follow-up care upon discharge. By fostering an environment where patients can receive dedicated support, we can better combat the cycle of hospitalization.
A Call for Future Research
Understanding the complexities of BPD and its management within inpatient settings calls for ongoing research. Future studies should explore the impact of systematic BPD-focused care and the effectiveness of various intervention protocols. By closely examining these variables, healthcare professionals can better tailor treatment strategies to mitigate the profound challenges faced by individuals diagnosed with BPD.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)