Unveiling the Hidden Risks of Ectopic Pregnancy in Assisted Reproductive Technology: A New Predictive Model
2025-03-28
Author: Ming
Introduction
Ectopic pregnancy (EP), the alarming condition where an embryo implants outside the uterus, is a serious complication that poses significant risks for women undergoing assisted reproductive technology (ART). Surprisingly, while ectopic pregnancies account for around 1% of maternal deaths in developing countries, the figure spikes to about 5% in more developed countries. Recent studies reveal that the rates of ectopic pregnancy following ART procedures vary widely, occurring in approximately 2.1% to 8.6% of cases, a stark contrast to the 1% to 2% incidence in natural pregnancies. This stark discrepancy underscores the critical need for improved predictive tools to anticipate and mitigate the risk of EP in ART patients.
Factors Affecting Ectopic Pregnancy Risk
Several factors have been linked to the risk of EP after ART, including tubal issues, abnormal body mass index (BMI), the type of embryo transfer (fresh or frozen), endometrial thickness, and the prevalence of polycystic ovary syndrome (PCOS). Understanding these risk factors more accurately could significantly enhance our ability to predict and prevent EP occurrences.
The Role of PCOS
Despite existing models aimed at forecasting risks related to ART, they often overlook significant variables like PCOS and BMI. Given PCOS's prevalence in women undergoing ART, integrating it into predictive models may provide a more nuanced risk assessment. PCOS is a common hormonal disorder affecting women of reproductive age and is a leading cause of infertility. Women with PCOS are prone to various pregnancy complications, both early and late-term, including pre-eclampsia and gestational diabetes, making the identification of risk factors vital for patient safety. The advent of ART has opened new avenues for PCOS patients desperate for motherhood; however, it has also introduced potential adverse effects such as miscarriage and ovarian hyperstimulation syndrome.
Recent Research Findings
One pivotal study has identified PCOS as a significant risk factor for ectopic pregnancy in the ART population by analyzing multiple risk indicators. This research contributes to the establishment of a novel prediction model that aims to minimize the incidence of EP, facilitating early detection and intervention.
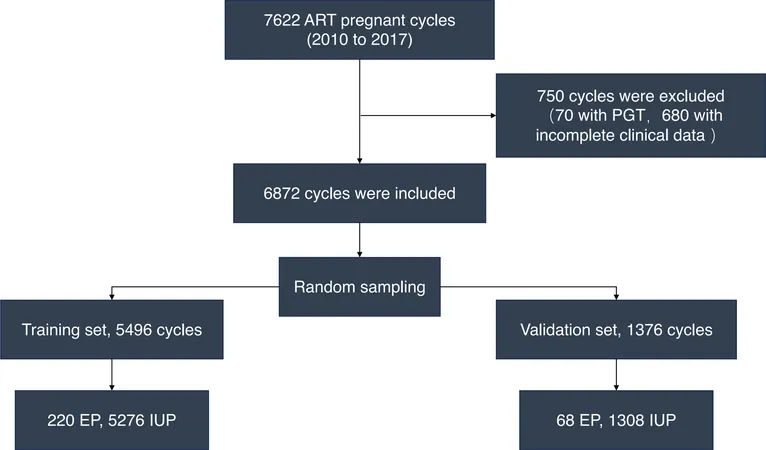
Study Methodology
The study in question was a retrospective cohort research conducted at the esteemed International Peace Maternal and Child Health Hospital. After meticulous selection, 6,872 ART cycles performed between 2010 and 2017 were analyzed, rigorously screening out cases with incomplete data or preimplantation genetic testing, and excluding subjects with certain endocrine dysfunctions. To determine risk factors for EP, the patients’ treatment protocols included controlled ovarian hyperstimulation (COH) using various regimens to monitor the ovarian response precisely, followed by embryo transfers tailored to patient conditions.
Results and Nomogram Development
The research focused on two primary outcomes: EP and intrauterine pregnancy (IUP). Data analysis affirmed that abnormalities in endometrial thickness (EMT), along with PCOS, significantly affected the rates of EP. Statistical analyses revealed that women with a history of ectopic pregnancy faced a heightened risk of recurrence, while fresh embryo transfers were notably linked to increased rates of ectopic occurrences. Moreover, increases in EMT were inversely associated with risk; each millimeter increase in EMT correlated with a reduced risk of EP. The study culminated in the development of a nomogram, a visual tool that combines various independent risk factors—like EMT, PCOS, history of EP, and types of embryo transfer—allowing practitioners to calculate the likelihood of EP in patients undergoing ART. The model demonstrated robust predictive power, showing remarkable stability in validation tests, promising a valuable resource for healthcare providers.
Conclusion and Future Directions
While the study highlights critical findings regarding the association between PCOS and EP risk—increasing the odds of EP in women with the condition by more than twofold—it acknowledges limitations, including the potential for unmeasured confounding factors and the homogeneity of the sample. Future multi-center and larger-scale studies will be essential to confirm these findings and refine predictive capabilities. Understanding the intricate relationship between PCOS, embryo transfer type, endometrial thickness, and the risk of ectopic pregnancy paves the way for more personalized medical approaches in ART. As in countless aspects of medicine, these insights not only promise to improve outcomes but could also save lives. Women embarking on the journey of motherhood through ART deserve safe, informed, and effective pathways to achieving their dreams.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)