Unveiling the Hidden Links Between Vaginal Microbes and Cervical Cancer: Are You at Risk?
2025-05-16
Author: Ming
The Startling Statistics of Cervical Cancer
Cervical cancer (CC) ranks as the fourth most common malignant tumor among women globally, with around 660,000 new cases and 350,000 deaths each year. Particularly alarming is its rising incidence in younger populations, especially in resource-limited regions, despite advancements in vaccination and screening.
The HPV Connection
Human papillomavirus (HPV) is highly associated with cervical cancer; types 16 and 18 account for nearly 70% of cases. Yet, most HPV infections don’t lead to cancer, pointing to other crucial elements like immune response, genetics, and the mysterious role of microorganisms in cancer development.
Microorganisms: The Silent Players in Cancer
Recent research reveals a compelling relationship between microorganisms and cancer. Roughly 15% of global cancer cases are linked to infectious agents, including various viruses and bacteria. Emerging evidence suggests that the vaginal microbiome, specifically its composition, may significantly influence the journey from HPV infection to cervical cancer.
Bacterial Vaginosis: A Risky Business
Bacterial vaginosis (BV), marked by an imbalance in the vaginal flora, has been linked to cervical cancer. Studies show that harmful bacteria prevalent in BV, such as Fusobacterium and Prevotella, might elevate the risk of cervical lesions, thus creating a more hospitable environment for HPV.
Exploring Microbial Diversity
Understanding the diversity of vaginal microbes becomes pivotal in assessing cancer risk. Specific microorganisms could either bolster or weaken the body’s defenses against HPV, leading to the persistence of infections and, consequently, cancer development. Supplementing with probiotics may alter the microbiome and potentially improve cancer treatment outcomes.
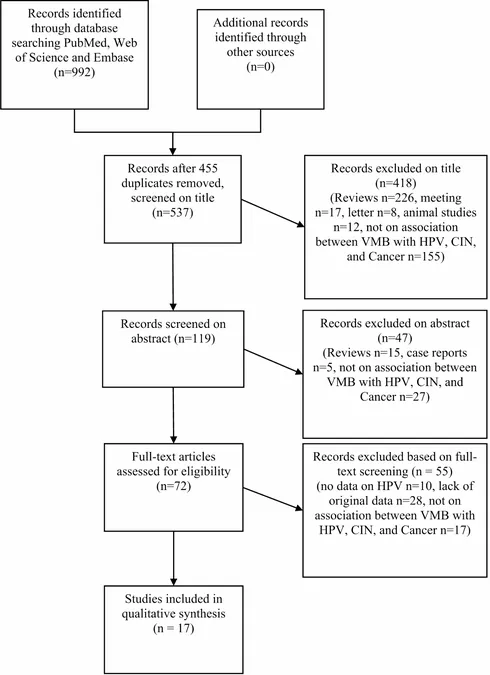
The Research Frontier: A Comprehensive Review
A systematic review aims to delve deeper into the links between vaginal microbiota (VMB) and cervical cancer. Researchers combed through extensive literature using high-throughput sequencing technologies to unravel how specific bacterial species relate to HPV status and cervical health.
Key Findings on Microbial Players
Analysis highlights the relative abundance of specific microorganisms—such as Prevotella and Sneathia—in patients with cervical cancer, suggesting their potential role in cancer progression. Remarkably, Prevotella was notably higher in CC patients compared to those without HPV infections.
The Need for Further Research
While the findings are illuminating, limitations such as geographic and ethnic biases underline the need for broader studies. Future research should rigorously explore how various factors—the host’s lifestyle, infections, and microbial variations—interact to influence cervical health.
A Call to Action: What Women Should Know
Understanding the complex relationships between vaginal microbiota and cervical cancer can empower women. Staying informed about sexual health, regular screenings, and potentially utilizing probiotic treatments could be essential steps in safeguarding against cervical cancer.
Conclusion: The Future of Cervical Cancer Prevention
As we continue to unravel the intertwining roles of microorganisms in cervical cancer, it becomes clear that a proactive approach in research, healthcare, and education is vital. By recognizing the potential risks and advocating for personal health, we can contribute to reducing the incidence of cervical cancer worldwide.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)