Unveiling the Hidden Link Between Lung Health and Arrhythmias: Groundbreaking Insights from Major Studies
2025-08-22
Author: Daniel
Study Overview: A Deep Dive into Cardiac and Pulmonary Interactions
In an innovative exploration of heart and lung health, research stemming from two robust cohort studies—the Atherosclerosis Risk in Communities (ARIC) study and The Cardiovascular Health Study (CHS)—has shed new light on the relationship between pulmonary function and arrhythmias. Initiated in the late 1980s, these extensive studies enrolled thousands of participants across various U.S. communities, aiming to tackle cardiovascular risks but inadvertently accumulating valuable arrhythmia data in the process.
A Closer Look at Participant Composition
The ARIC study began with 15,792 participants aged between 45 and 64 years, while CHS included adults aged 65 and older. The combined analytical cohort totaled 17,684 individuals, with a significant representation of women (54.2%) and men (45.8%). To ensure the reliability of the findings, participants were rigorously screened for baseline cardiac arrhythmias and other confounding factors.
The Vital Role of Lung Function in Arrhythmias
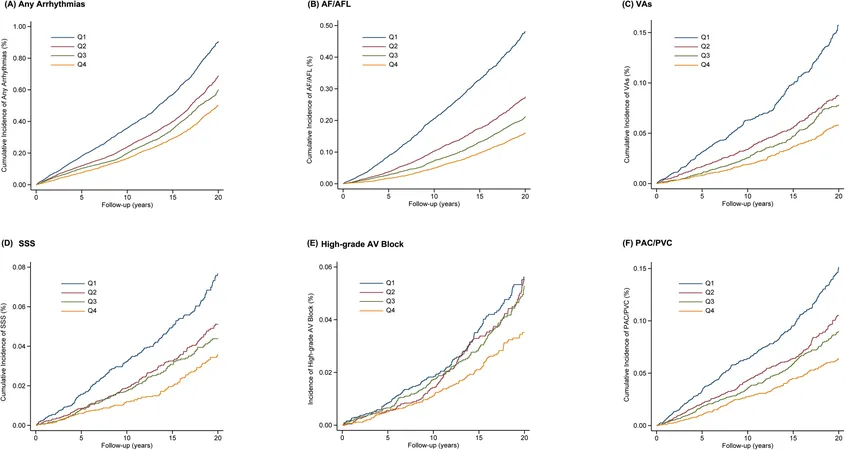
This groundbreaking research focused on key pulmonary function metrics—FEV1%, FVC%, and the FEV1/FVC ratio—assessing how variations in these parameters correlated with the incidence of various arrhythmias. Not surprisingly, diminished lung function emerged as a significant predictor of higher arrhythmia risk, particularly among individuals with obstructive and restrictive lung disease patterns.
Risk Disparities Across Demographics
Results indicated a striking pattern: those in the lowest quartile of lung function experienced a substantially higher risk of any arrhythmia compared to their healthier counterparts. Notably, race played a pivotal role, with White participants exhibiting greater sensitivity to the impacts of reduced lung function on arrhythmia risks compared to Black participants.
Unraveling the Mechanisms: How Does Lung Health Affect Heart Rhythm?
The researchers propose a triad of mechanisms that could explain these associations: 1. **Chronic Inflammation**: Lung impairment may trigger systemic inflammation, potentially igniting arrhythmogenic processes. 2. **Autonomic Dysregulation**: Abnormalities in the autonomic nervous system due to lung diseases may increase cardiac electrical instability. 3. **Pulmonary-Ventricular Interaction**: Changes in pulmonary circulation due to lung disease could lead to alterations in heart structure and function.
Key Findings: The Data Speaks
With over 7408 cases of arrhythmias documented during a median follow-up of 12.6 years, this research presents definitive evidence linking lung function impairment to various arrhythmias, including atrial fibrillation and ventricular tachycardia. Each decline in lung function parameter directly correlated with an increase in arrhythmic events, underscoring the need for proactive pulmonary assessments in at-risk populations.
Moving Forward: A Call for Comprehensive Approaches to Health
These findings are pivotal, suggesting that lung health is not merely a separate entity but intricately connected to cardiac well-being. This research advocates for a more integrated approach to health assessments, emphasizing the necessity for early identification of pulmonary issues as a strategy to mitigate arrhythmia risks.
Conclusion: A New Paradigm in Cardiac Risk Assessment
As we advance into an era focused on holistic healthcare, understanding the interdependence between lung function and cardiac rhythm is crucial. The insights from ARIC and CHS dare us to rethink how we approach both pulmonary and cardiovascular health, positioning lung function as a critical component in the prevention of cardiac arrhythmias.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)