Unveiling Self-Management Trends in Chronic Heart Failure Patients: A Yearlong Study
2025-04-29
Author: Daniel
The Heart of the Matter: Understanding Chronic Heart Failure
Chronic heart failure (CHF) affects approximately 26 million people worldwide, with about 8.9 million cases reported in China alone. This condition markedly escalates morbidity and mortality rates, translating into hefty medical costs and significant caregiver burden. Older patients, especially, face heightened risks of hospital readmission due to deterioration in cardiac function, compounded by other coexisting health issues.
Self-Management: A Lifesaver for CHF Patients
Self-management stands out as a crucial intervention for CHF patients, enabling them to manage symptoms and embrace lifestyle changes effectively. Studies indicate that enhancing self-management skills can boost both quality of life and mental health, ultimately curbing readmissions.
A Gap in Knowledge: The Need for Longitudinal Studies
Despite the importance of self-management, existing research is predominantly cross-sectional, often overlooking how these behaviors evolve over time. This study aims to fill that void by examining the self-management levels of CHF patients at multiple intervals post-discharge—1, 3, 6, and 12 months.
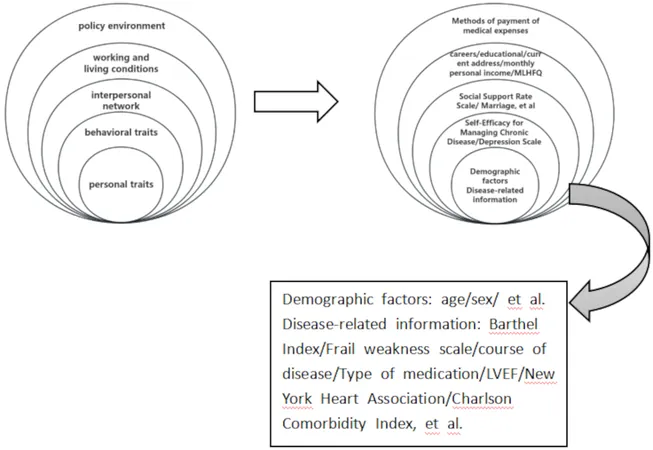
Using the Health Ecological Model: A Comprehensive Framework
The Health Ecological Model serves as the theoretical backdrop for this study, suggesting that individual health is influenced by a blend of personal traits and environmental factors. This research intends to identify various influencing factors on self-management to help clinicians devise targeted interventions.
Research Mechanics: Who Participated?
From December 2021 to June 2022, older patients hospitalized with CHF at a leading hospital in Yinchuan were included in a longitudinal study. Inclusion required participants to be 60 or older, have appropriate cognitive function, and consent to participate.
Unveiling Findings: The Journey of Self-Management Over Time
Data from 213 patients, including their demographic information and health conditions, led to profound insights. Self-management scores displayed a dynamic shift, peaking just one month post-discharge but revealing a significant decline by three months. This pattern exposes crucial timelines when patient follow-up is necessary.
Factors Affecting Self-Management: Who’s Influencing What?
The study found that education level, social support, and self-efficacy are pivotal in determining self-management behaviors. Higher levels of education and income correlate with better self-care practices, while robust social support significantly enhances patient adherence to self-management.
Depression and Quality of Life: The Unseen Tug-of-War
Interestingly, while depression and quality of life were linked to self-management scores, they did not emerge as independent determinants. This suggests a complex interplay between mental well-being and health management practices, emphasizing the need for tailored psychotherapeutic strategies in chronic disease care.
Looking Ahead: Enhancing Self-Management Interventions
As the study highlights the challenges and factors influencing self-management among CHF patients, it reinforces the necessity for continued education and resource allocation. Medical staff must prioritize empowering patients during vulnerable times—with an emphasis on psychological support to foster better health outcomes.
Conclusion: The Road to Improved Heart Health
This longitudinal study navigates the self-management landscapes of CHF patients and pinpoints essential elements that could improve quality of life. By understanding trends and implementing targeted strategies, healthcare providers can significantly enhance the management of chronic heart conditions, fostering better health advantages long-term.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)