Unraveling the Sleep Struggles: Insomnia and its Links to Schizophrenia
2025-08-28
Author: Siti
Schizophrenia—a debilitating psychiatric disorder—affects millions worldwide, characterized by cognitive dysfunction, delusions, hallucinations, and chaotic behavior. In China alone, its lifetime prevalence reaches 0.7%, presenting significant social and occupational challenges, not to mention a staggering disability burden.
Among the many issues faced by individuals living with schizophrenia, insomnia stands out, impacting up to 80% of patients across various studies. Sleep difficulties are not just an occasional annoyance but a persistent problem felt throughout different stages of the illness, with insomnia often peaking even in chronic phases.
Interestingly, a recent survey highlighted that schizophrenia patients receiving primary care had insomnia rates significantly higher than the general populace, indicating deep-rooted challenges that persist even when psychiatric symptoms stabilize. Comorbid insomnia substantially worsens cognitive function, diminishes quality of life, and heightens suicidal tendencies, underscoring an urgent need to understand its complexities.
The Disturbing Connection: Psychotic Symptoms and Insomnia
Insomnia in schizophrenia patients isn’t purely incidental. Research has shown a striking correlation between various psychotic symptoms—especially hallucinations—and sleep disturbances. These psychotic features can trigger and worsen insomnia, creating a vicious cycle where poor sleep exacerbates symptoms like delusions and mood swings, leading to further sleep issues.
Moreover, chronic sleep deprivation can derail cognitive functions and emotional stability, crafting a challenging feedback loop detrimental to overall well-being.
Depressive Symptoms: The Silent Contributor to Insomnia
Adding to the insomnia puzzle are depressive symptoms, found in approximately 28.6% of those with schizophrenia. These symptoms significantly disrupt sleep quality, acting as a predictor for persistent insomnia. As depression intertwines with psychotic symptoms, patients often face a compounded struggle, demanding careful clinical attention.
The Role of Biological Mechanisms in Sleep Disruption
Sleep disturbances may also stem from intricate biological mechanisms beyond clinical symptoms. Many schizophrenia patients exhibit metabolic dysfunction, notably concerning glucose and lipid metabolism, which can adversely affect sleep. Studies indicate that those with metabolic disorders report poorer sleep quality, revealing a complex interaction between biological health and sleep.
Emerging research suggests inflammatory processes could play a pivotal role in the development and severity of insomnia. Multiple clinical findings tie sleep issues to dysregulated inflammatory markers, with higher levels of cytokines like IL-6 linked to poorer sleep outcomes.
Urgent Need for Comprehensive Research
Despite initial insights into insomnia within schizophrenia, discrepancies in research findings remain. Current literature presents varied results regarding the correlation between insomnia and clinical characteristics, often overlooking deeper biological factors like inflammatory and lipid metabolism markers.
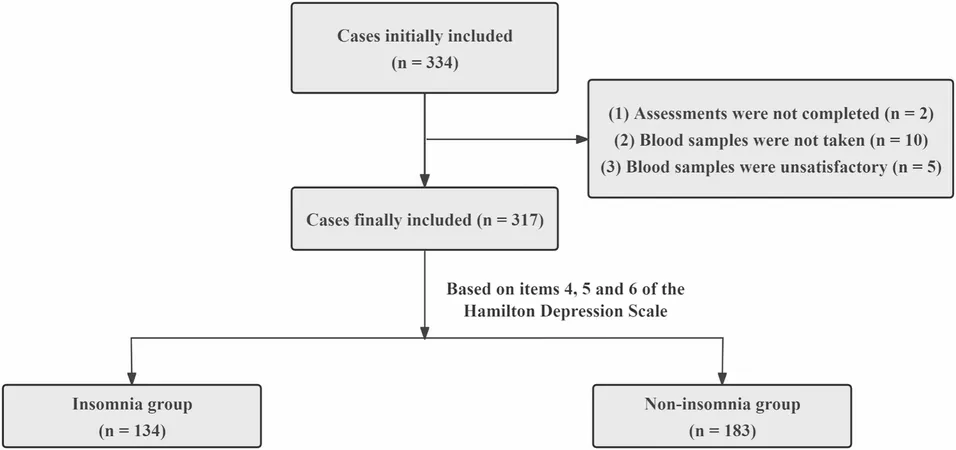
To fill these gaps, a new cross-sectional study was conducted to gather prevalence data on insomnia among chronic schizophrenia patients while analyzing its correlations with clinical features and blood biomarkers.
Research Overview and Collection Methods
This comprehensive study, conducted across three major hospitals in Anhui, China, focused on chronic schizophrenia patients. With careful screening criteria, researchers sought to document insomnia prevalence while analyzing potential biological markers that may link insomnia to inflammation and metabolic dysregulation.
Measuring tools were deployed to assess a range of factors—including sociodemographic data, sleep quality through the Hamilton Depression Rating Scale, and serum lipid levels—leading to data analysis that revealed a troubling 42.3% of patients report insomnia symptoms.
Sociodemographic Linkages and Clinical Insights
Findings suggest older age correlates with higher insomnia rates, potentially due to biological shifts in sleep rhythms coupled with psychosocial factors like isolation or loss. Additionally, intense psychotic symptoms persist as significant contributors to sleep issues, demanding clinical interventions tailored to alleviate these intertwined symptoms.
Moreover, the interplay of depressive symptoms with psychotic features intensifies sleep disturbances, reinforcing the necessity for targeted therapeutic approaches. Innovative treatment options, including cognitive behavioral therapy and pharmacological solutions, have shown promise in improving both depressive symptoms and sleep quality.
Unpacking Inflammation's Role in Sleep Quality
Interestingly, this study's results highlighted high IL-6 levels as a potential independent risk factor for insomnia. Given the established link between inflammation and sleep disruption, this could offer new pathways for early intervention strategies aimed at insomnia management in chronic schizophrenia cases.
In contrast, the study did not find strong evidence linking lipid metabolism with insomnia, demonstrating a need for further exploration into this complex relationship.
Conclusion: A Call for Future Research and Interventions
In conclusion, this research underscores the critical interplay of clinical features, unique biological markers, and psychological components contributing to insomnia in chronic schizophrenia. As we navigate this intricate web, it becomes clear that comprehensive strategies addressing both mental health symptoms and associated biological factors are essential in improving sleep quality and overall patient outcomes.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)