Unraveling the Mystery of Diabetic Pain: How Forgotten Cell Clusters Could Transform Treatment
2025-05-12
Author: Ming
A Century-Old Discovery Gains New Relevance
In a groundbreaking study from The University of Texas at Dallas's Center for Advanced Pain Studies, researchers are bringing a century-old phenomenon back into the spotlight. Known as Nageotte nodules, these enigmatic cell clusters may hold vital insights into the debilitating pain caused by diabetic neuropathy.
Nageotte Nodules: A Key to Understanding Neuropathic Pain
Recent research published in Nature Communications indicates that these Nageotte nodules could be a crucial indicator of nerve cell deterioration in human sensory ganglia. Dr. Ted Price, an expert in neuroscience and director of the Center, points to this discovery as a potential game-changer in how we perceive and treat diabetic pain. "Our findings challenge existing views of diabetic neuropathic pain and highlight neurodegeneration in the dorsal root ganglion as a critical element of the condition," he stated.
The Alarming Scope of Diabetic Neuropathy
Diabetic neuropathy is one of the most prevalent types of neuropathic pain, impacting around 11 million Americans—nearly a third of the 38 million diabetes sufferers in the country. The condition often strikes in the extremities, leading to sharp, debilitating pain that can severely affect quality of life.
Mapping Human Pain Mechanisms: A New Frontier
To better understand pain mechanisms, Dr. Stephanie Shiers and her team at CAPS are delving into the anatomy of human dorsal root ganglia and other sensory tissues. Their groundbreaking research revealed that Nageotte nodules appear more frequently in diabetes patients, especially those suffering from diabetic neuropathy. This new data is poised to shift how scientists approach pain management.
Rediscovering Nageotte Nodules: A Historical Oversight?
Originally identified in rabbits by French neuroanatomist Jean Nageotte in 1922, these nodules have been largely overlooked for the past 100 years. Shiers’ investigation shows that these dead sensory neurons transform into clusters of non-neuronal cells, revealing how high blood sugar levels may compromise neuron viability. Until now, very little has been documented about their molecular structure or their link to pain.
The Unique Pathology of Diabetic Sensory Neurons
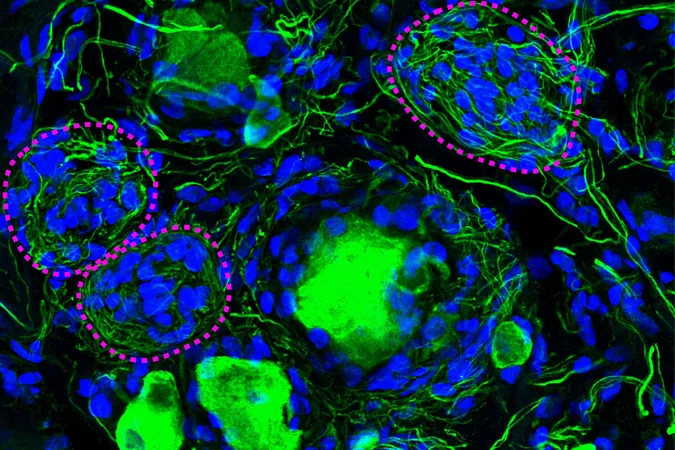
In her study, Shiers and her colleagues utilized advanced histology and spatial sequencing techniques to analyze the molecular characteristics of Nageotte nodules. Surprisingly, they found these nodules teeming with satellite glia and non-myelinating Schwann cells intertwined with bundles of sensory neuron axons—a condition not previously documented in humans.
A New Outlook on Treatment Possibilities
Shiers hypothesizes that spontaneous activity within these atypical fibers could be the culprit behind diabetic neuropathy. Furthermore, her research, which includes samples from 90 individuals—in stark contrast to earlier studies focused on single cases—opens new doors to understanding not just diabetic neuropathy but broader neuropathic conditions.
The Importance of Collaborative Research
This innovative research is made possible thanks to the efforts of the Southwest Transplant Alliance, a nonprofit dedicated to organ recovery. Their role in providing organ donors for these studies is invaluable, with President and CEO Brad Adams emphasizing the hope these findings bring to families who have donated organs.
Charting New Territory in Pain Research
Dr. Price and his team believe that this research signifies a pivotal shift in our understanding of sensory neurons and their role in pain. The identification of Nageotte nodules may not only enhance our insights into diabetic neuropathy but could also pave the way for new treatment strategies, offering a glimmer of hope to millions dealing with chronic pain.





 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)